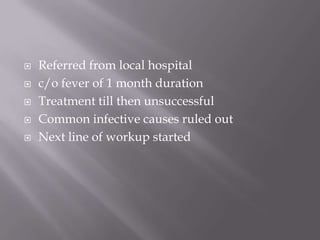
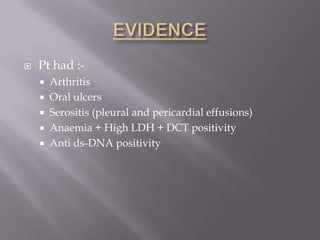
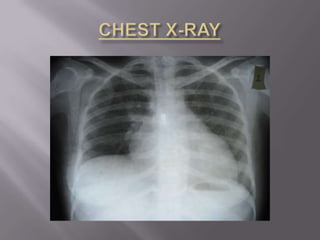
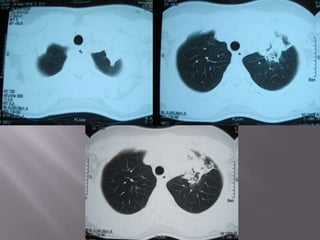
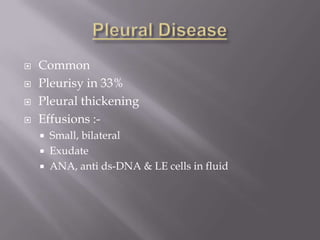
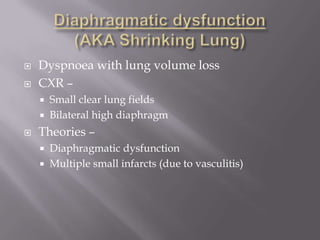
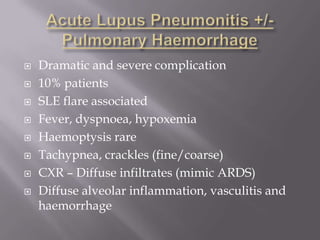
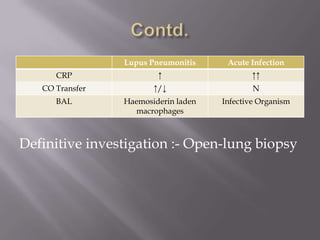
This document discusses the case of a 31-year-old woman referred for fever of 1 month duration. She was diagnosed with systemic lupus erythematosus based on her symptoms and test results. She developed new onset cough and chest pain while being treated with steroids. Imaging showed consolidation and effusions. Antibiotics did not improve her symptoms, shifting suspicion to lupus pneumonitis. Increasing steroids dosage resolved her symptoms. The document then provides an overview of lupus pneumonitis, its presentation, diagnostic evaluation and treatment.