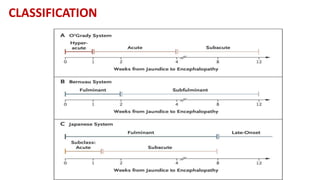
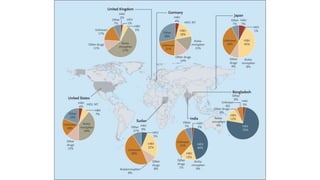
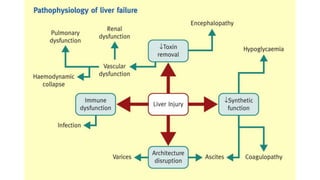
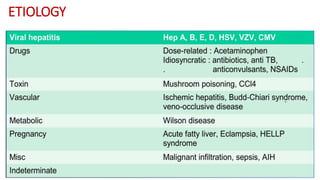
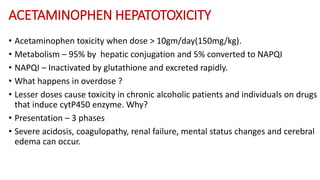
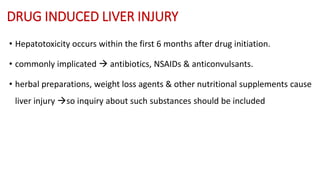
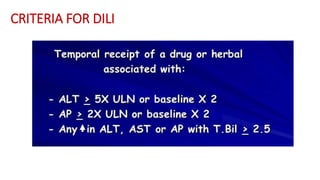
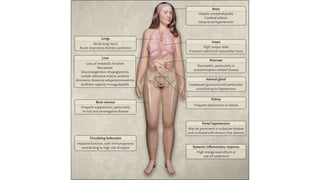
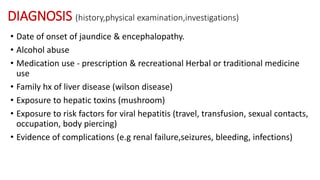
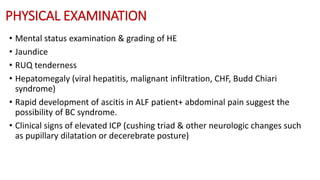
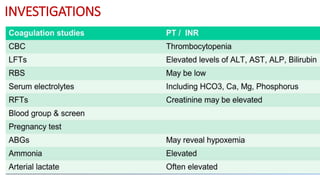
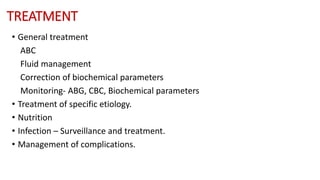
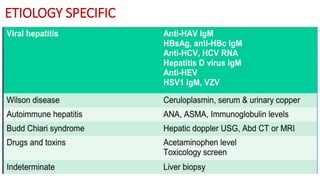
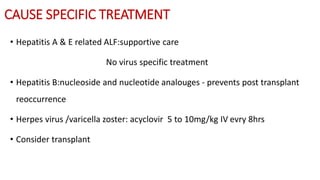
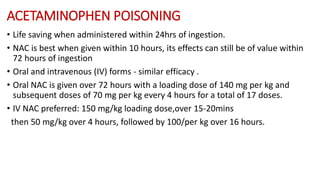
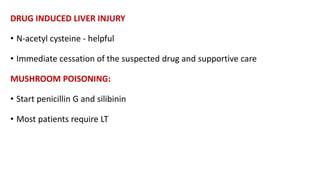
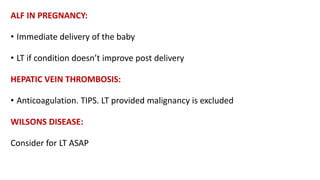
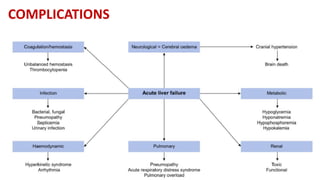
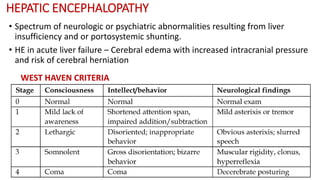
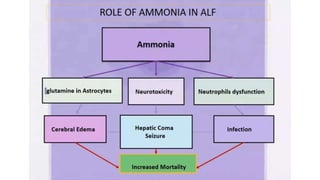
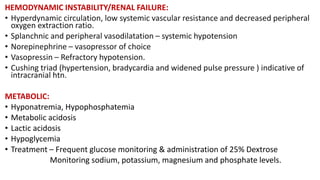
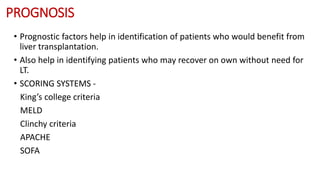
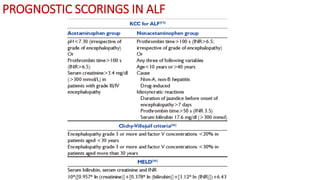
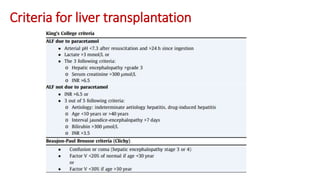
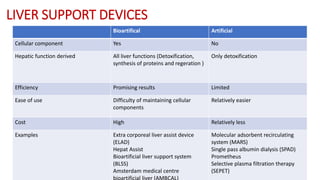
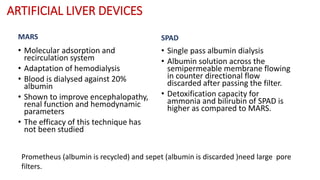
This document provides an overview of acute liver failure (ALF), including its definition, classification, etiology, clinical manifestations, diagnosis, treatment, complications, prognosis, and liver support devices. ALF is defined as evidence of coagulation abnormalities and mental alterations in a patient without preexisting cirrhosis within 26 weeks of illness onset. Common etiologies in India include hepatitis E, drug-induced liver injury, and acetaminophen toxicity. Presentation may include jaundice, coagulopathy, and hepatic encephalopathy. Treatment involves supportive care and managing complications such as cerebral edema. Prognosis is assessed using scoring systems like King's College criteria, with liver transplantation indicated for those who do not recover spontaneously.
![DEFINITION
• Evidence of coagulation abnormalities (international normalized ratio [INR]
>1.5) and mental alterations (encephalopathy) of a patient without
preexisting cirrhosis and <26 weeks of illness duration .](https://image.slidesharecdn.com/acuteliverfailure-230111115302-6324c6d3/85/Acute-liver-failure-pptx-3-320.jpg)