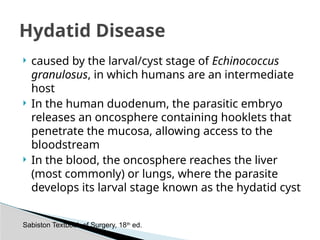
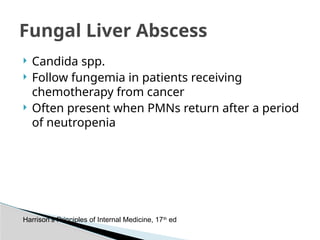
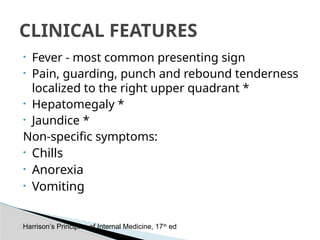
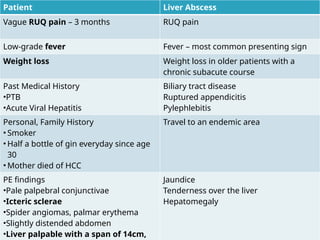
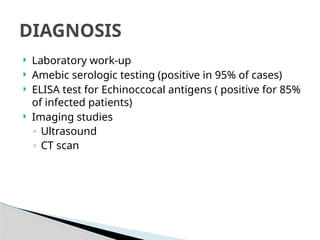
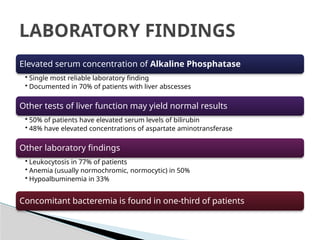
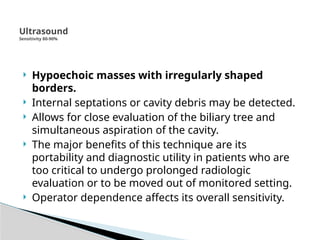
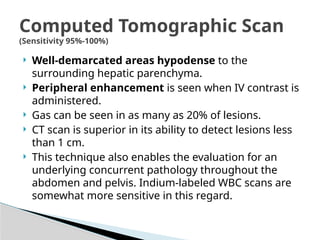
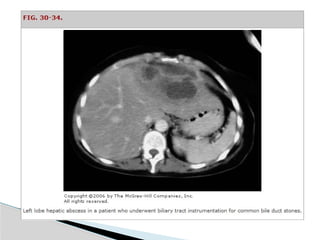
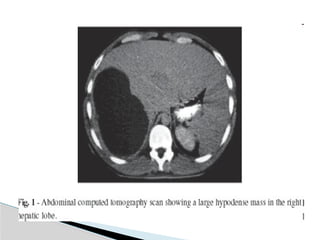
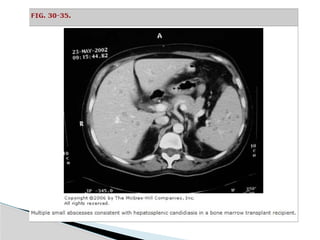
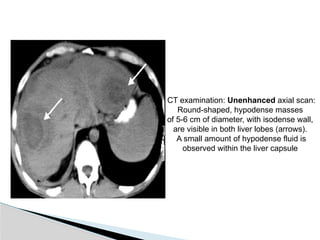
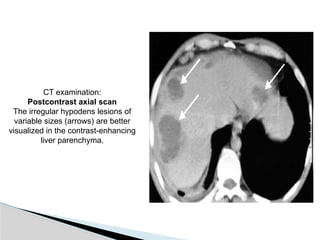
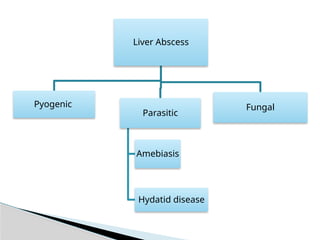
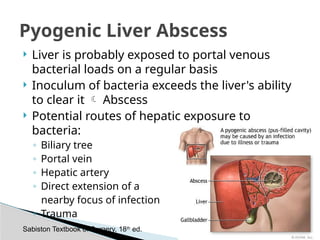
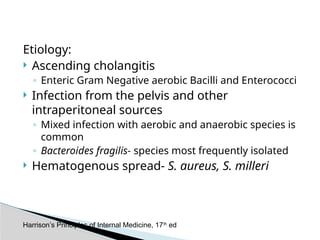
Liver abscesses can arise from various infections, primarily affecting the right hepatic lobe due to anatomical factors. Clinical features vary by type, with pyogenic abscesses often presenting with fever and abdominal pain, while amebic abscesses may show elevated amebic serology and are more common in younger patients. Diagnosis typically involves serologic testing, imaging studies, and management options include percutaneous drainage and medical therapy based on the underlying cause.


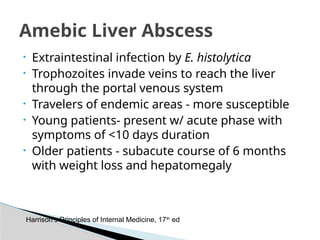
![CLINICAL FEATURES AMEBIC ABSCESS PYOGENIC ABSCESS
Age (yr) 20-40 >50
Male-to-female ratio ≥10:1 1.5:1
Solitary vs. multiple Solitary 80%[*]
Solitary 50%
Location Usually right liver Usually right liver
Travel in endemic area Yes No
Diabetes Uncommon (∼2%) More common (∼27%)
Alcohol use Common Common
Jaundice Uncommon Common
Elevated bilirubin Uncommon Common
Elevated alkaline
phosphatase
Common Common
Positive blood culture No Common
Positive amebic serology Yes No
Table 52-5 -- Features of Amebic Versus Pyogenic Liver Abscess
Sabiston Textbook of Surgery, 18th
ed.](https://image.slidesharecdn.com/6005450-240907170425-9a7809ff/85/A-liver-abscess-presentation-for-mbbs-ppt-9-320.jpg)