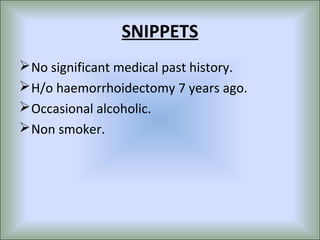
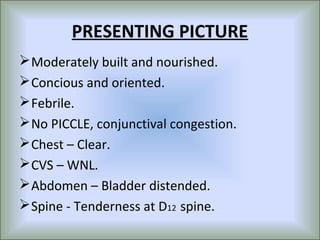
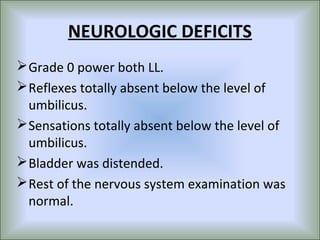
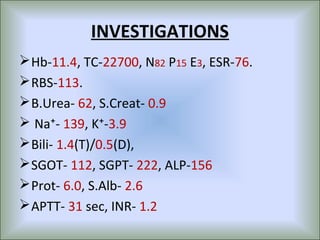
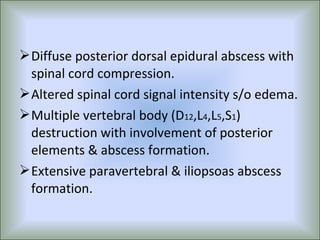
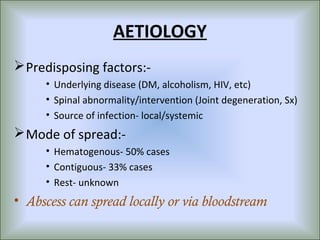
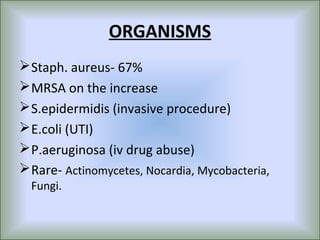
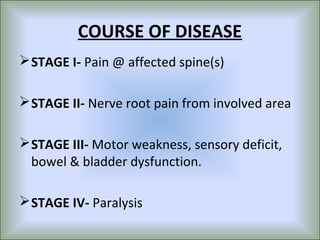
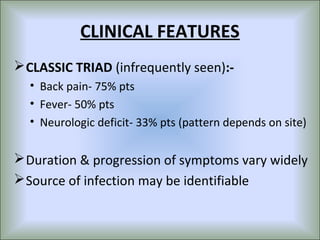
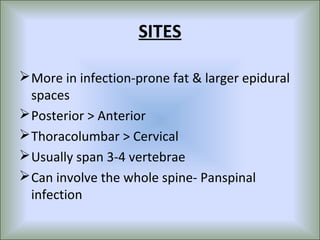
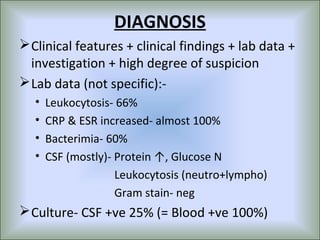
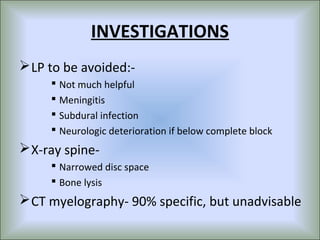
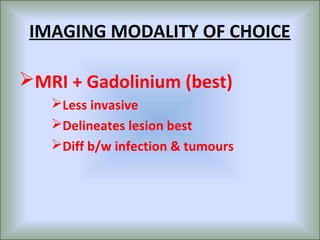
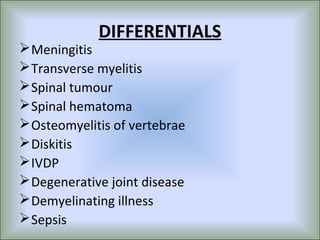
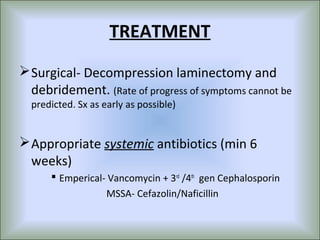
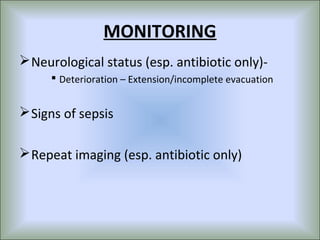
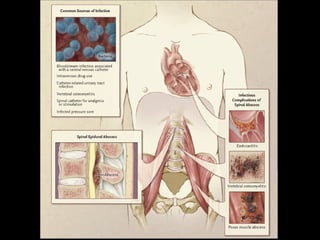
This document describes a case of spinal epidural abscess in a 28-year-old man. He developed back pain that progressed to weakness and loss of sensation in his lower limbs. Imaging showed an epidural abscess involving several vertebrae. He underwent surgery to drain the abscess and was treated with antibiotics. Histopathology confirmed tuberculosis. He showed improvement in strength after treatment but was discharged with some residual weakness. The document also provides an overview of spinal epidural abscess, including causes, clinical features, diagnosis, treatment and prognosis.