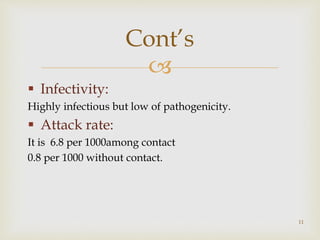
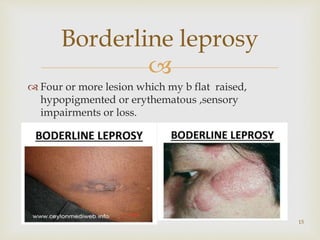
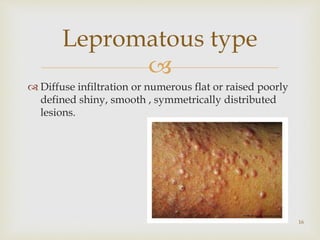
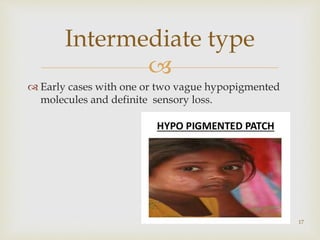
This document provides an overview of leprosy, including its definition, epidemiology, signs and symptoms, treatment, and control measures. It defines leprosy as an infectious disease caused by Mycobacterium leprae, characterized by hypopigmented patches and loss of sensation. The presentation discusses the distribution of leprosy by time, place, and person. It also covers the disease's classification, pathophysiology, clinical features, diagnosis, complications, and treatment options involving multidrug therapy. The document concludes by outlining various methods for leprosy control, such as surveillance, early detection, chemotherapy, and health education.