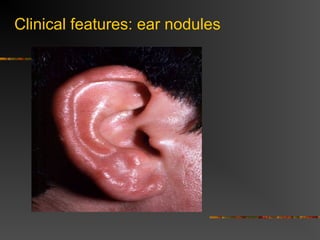
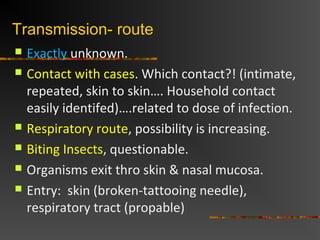
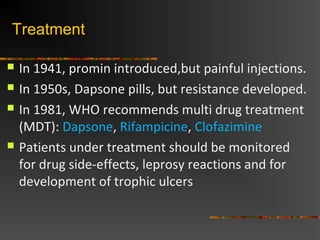
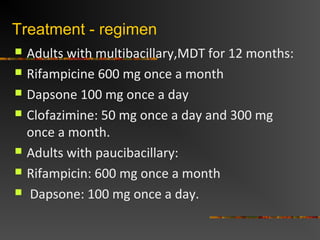
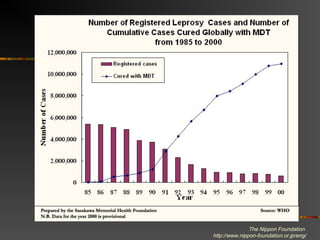
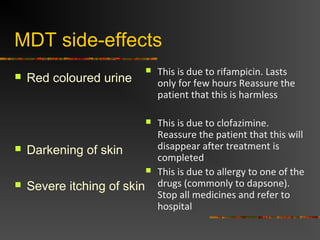
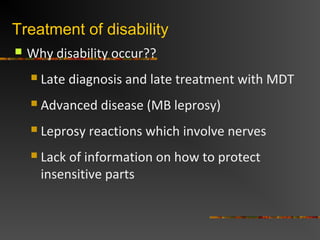
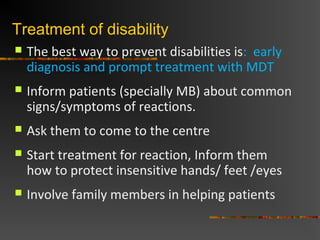
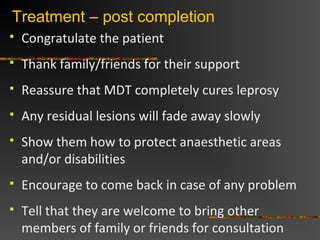
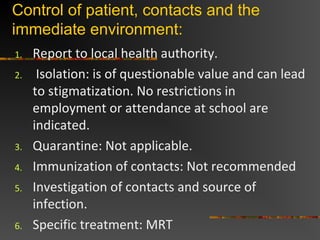
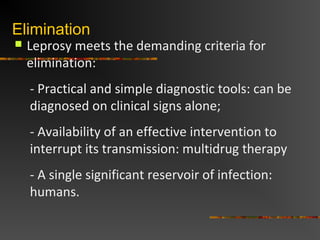
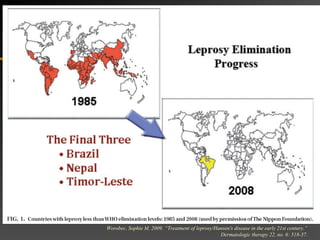
Leprosy is caused by Mycobacterium leprae, an acid-fast bacillus. It primarily affects the skin and peripheral nerves, causing sensory loss and disability if left untreated. While only a small portion of those exposed develop clinical disease, transmission occurs through droplets from the nose and mouth. Treatment involves multidrug therapy with dapsone, rifampicin, and clofazimine, which cures the disease and eliminates infectivity. Control relies on early diagnosis and treatment to prevent disability, along with health education to reduce stigma. Global efforts have led to the elimination of leprosy as a public health problem.