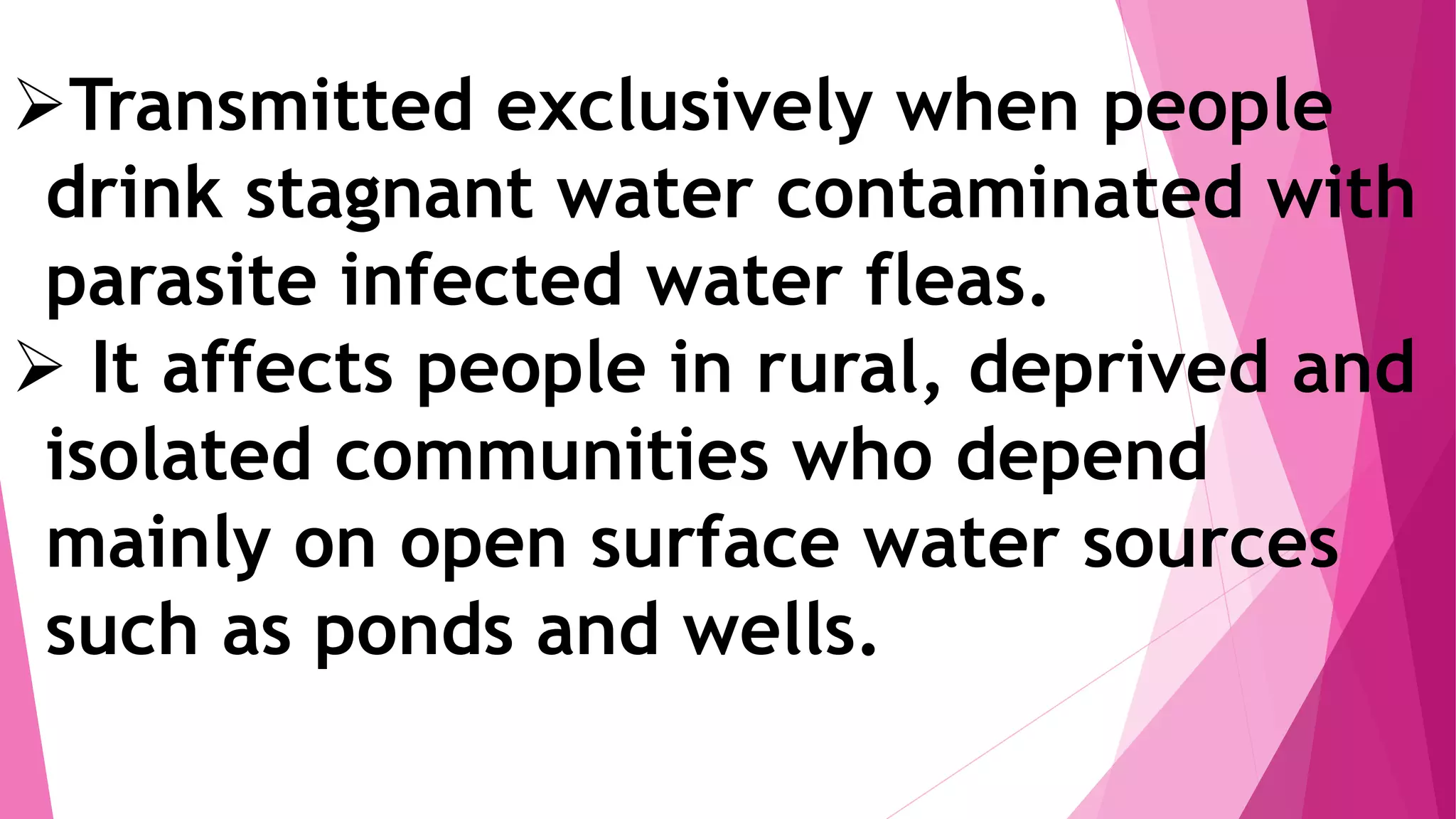
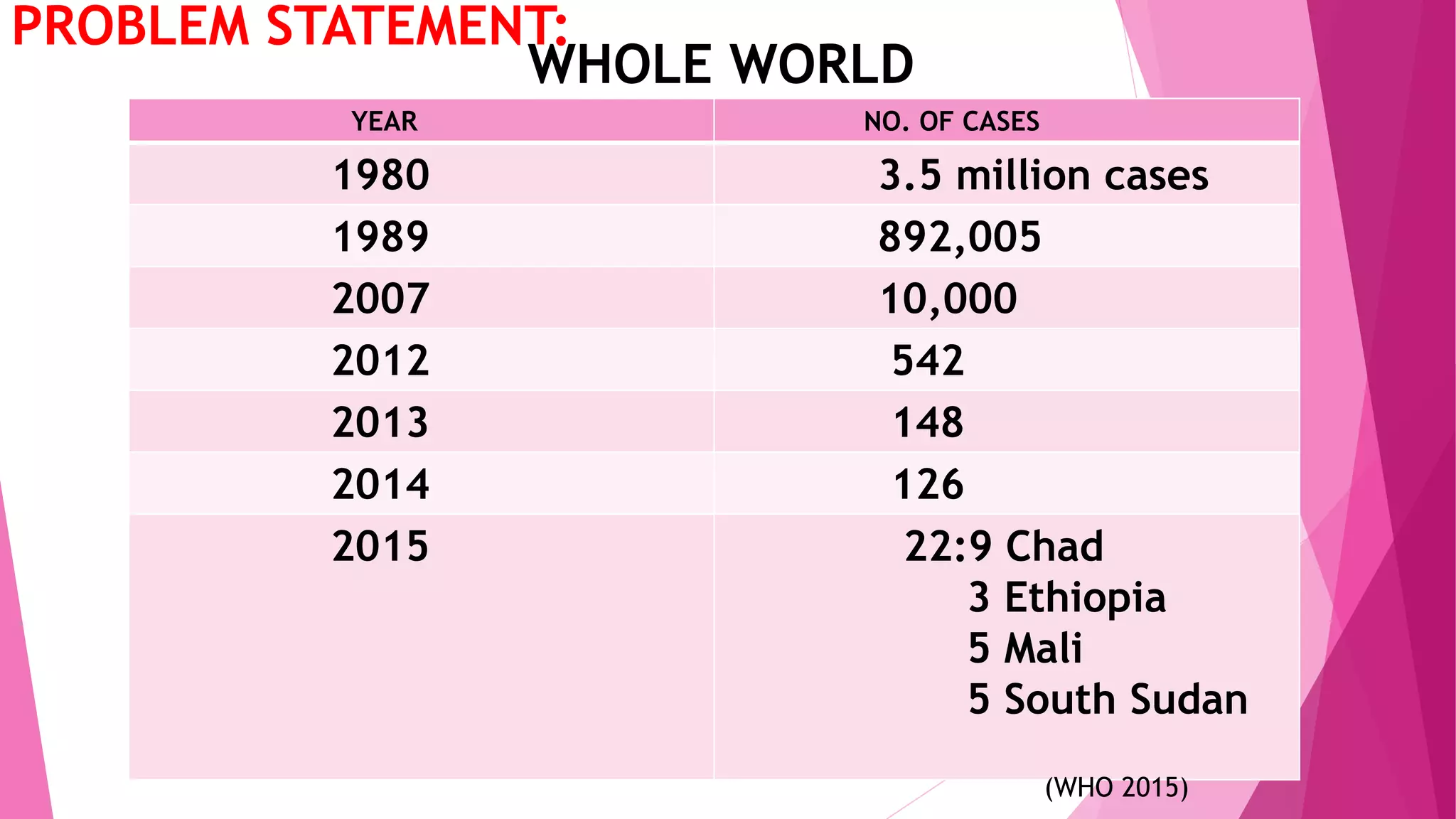
Dracunculiasis, also known as guinea worm disease, is caused by the nematode Dracunculus medinensis. It is transmitted when people drink water contaminated with water fleas infected with Dracunculus medinensis larvae. The larvae mature and emerge slowly from blisters on the skin after about a year, causing intense pain. Prevention focuses on filtering drinking water and preventing people with emerging worms from contaminating water sources. India launched a national eradication program in 1984 and was certified guinea worm free in 2000 after three years of zero reported cases. Surveillance continues to ensure guinea worm disease does not reemerge.