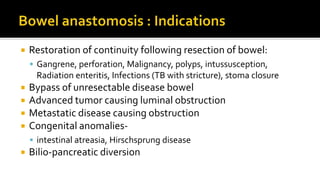
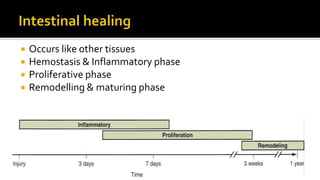
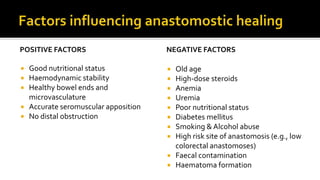
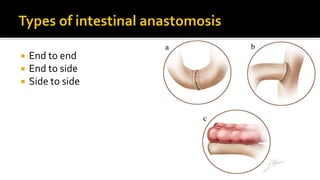
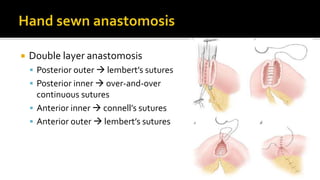
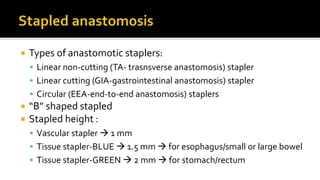
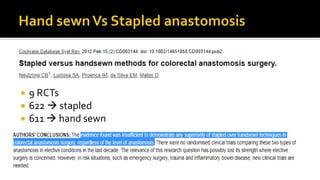
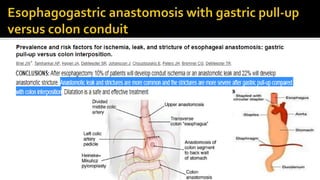
This document discusses intestinal anastomosis, which involves creating a connection between intestinal loops or ends. Intestinal anastomosis is commonly performed for elective and emergency cases involving conditions like cancer, infections, or obstructions. The key factors for a successful anastomosis are minimal contamination, good blood supply, and tension-free apposition of the intestinal ends. The document compares hand-sewn and stapled techniques, noting that while staplers are faster, studies have found no difference in outcomes between the two methods. Proper patient factors and surgical technique are more important than the specific method used.