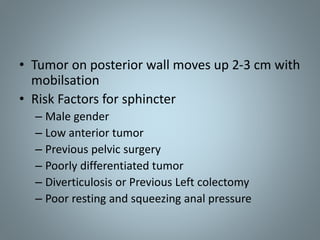
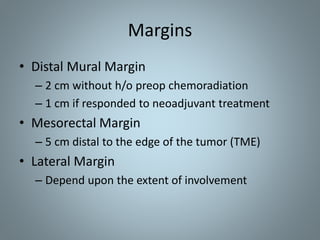
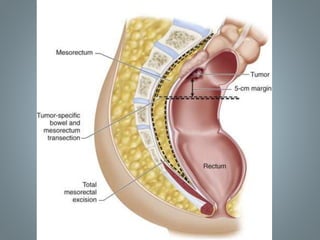
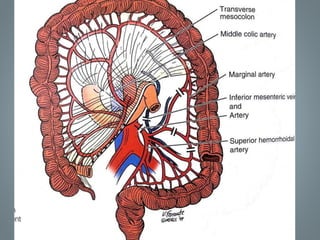
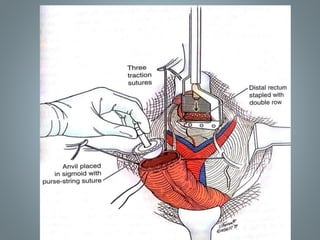
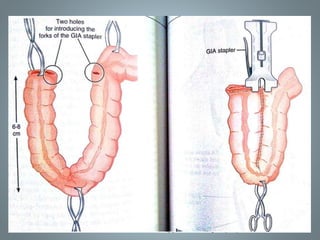
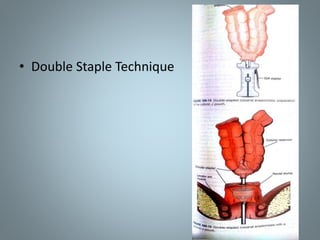
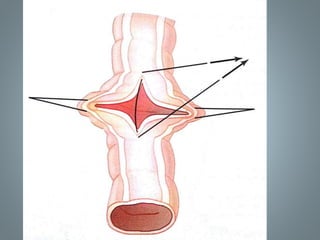
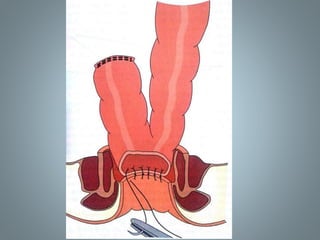
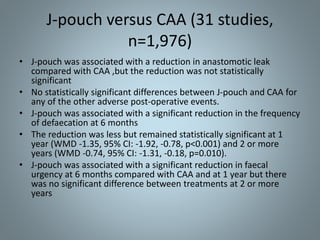
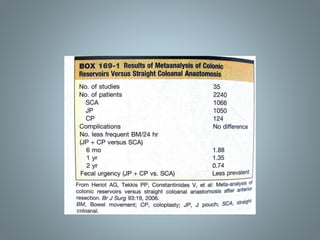
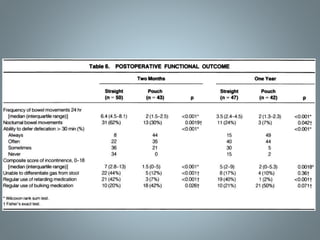
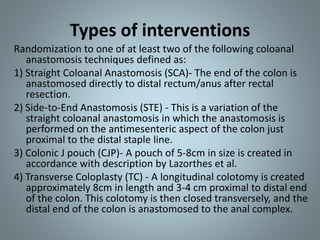
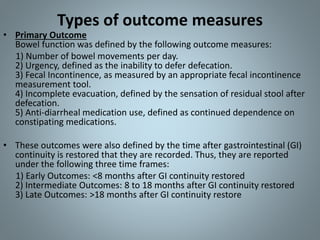
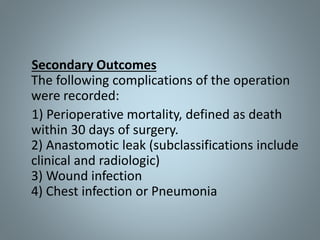
The document discusses various reconstruction methods after low anterior resection (LAR) for rectal cancer, comparing techniques such as straight coloanal anastomosis, colonic J-pouch, and transverse coloplasty. It highlights the advantages of colonic J-pouch in terms of bowel function and reduced anastomotic leakage, particularly in the first few months post-operation, while encouraging further research on alternatives like transverse coloplasty and side-to-end anastomosis. Recommendations suggest that colonic J-pouch should be preferred due to better clinical outcomes, although more comprehensive studies are needed for other techniques.