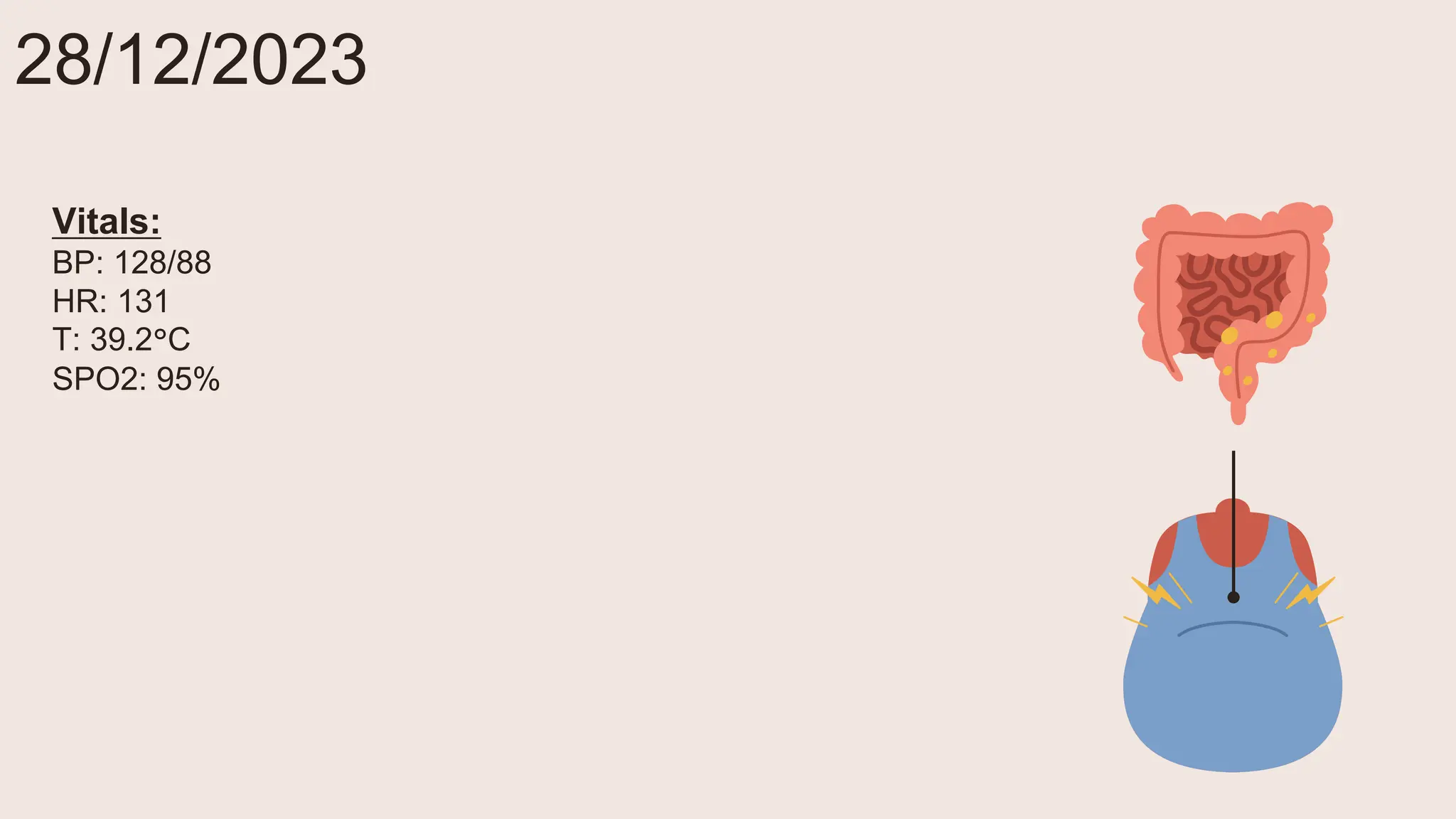
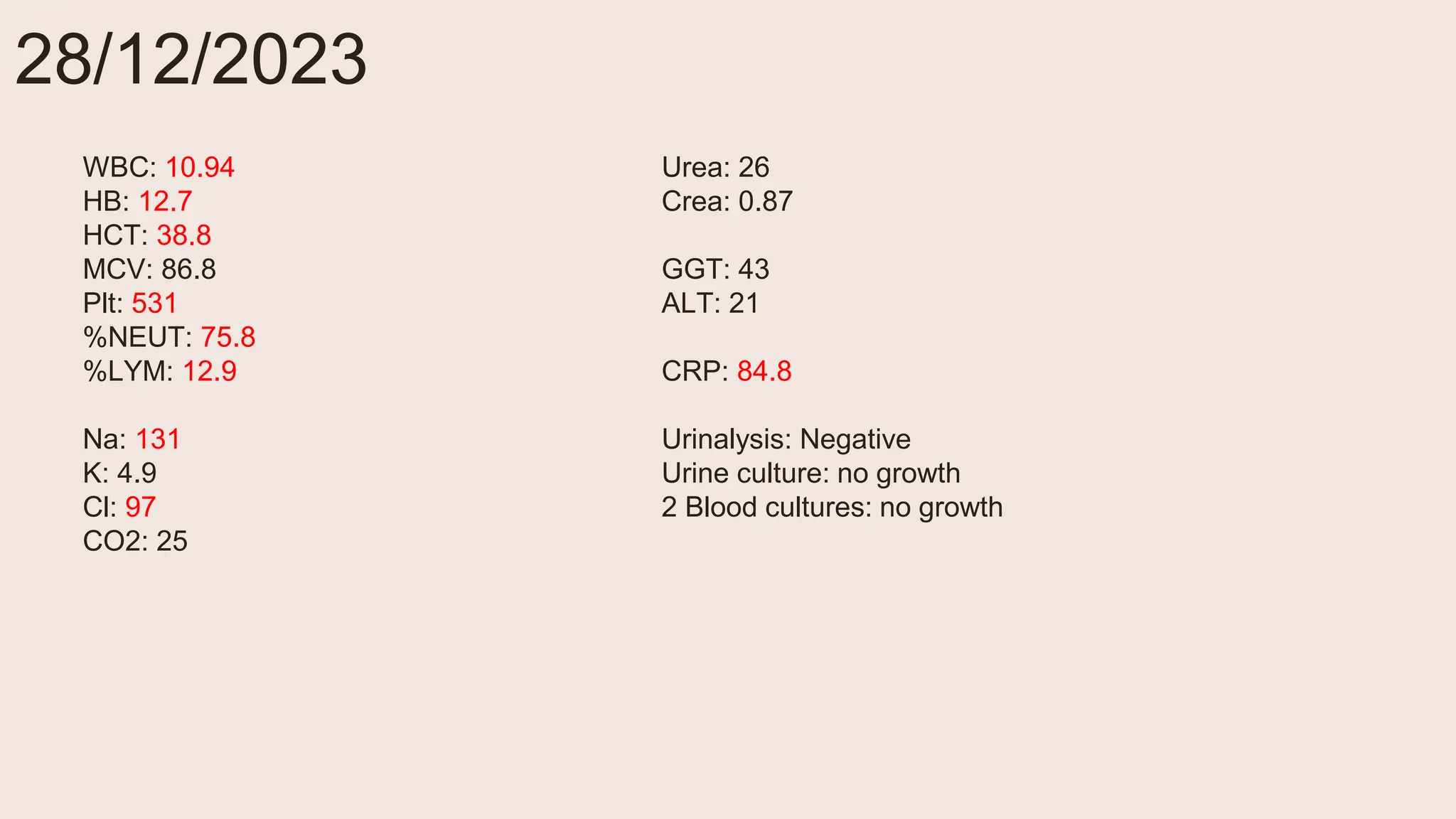
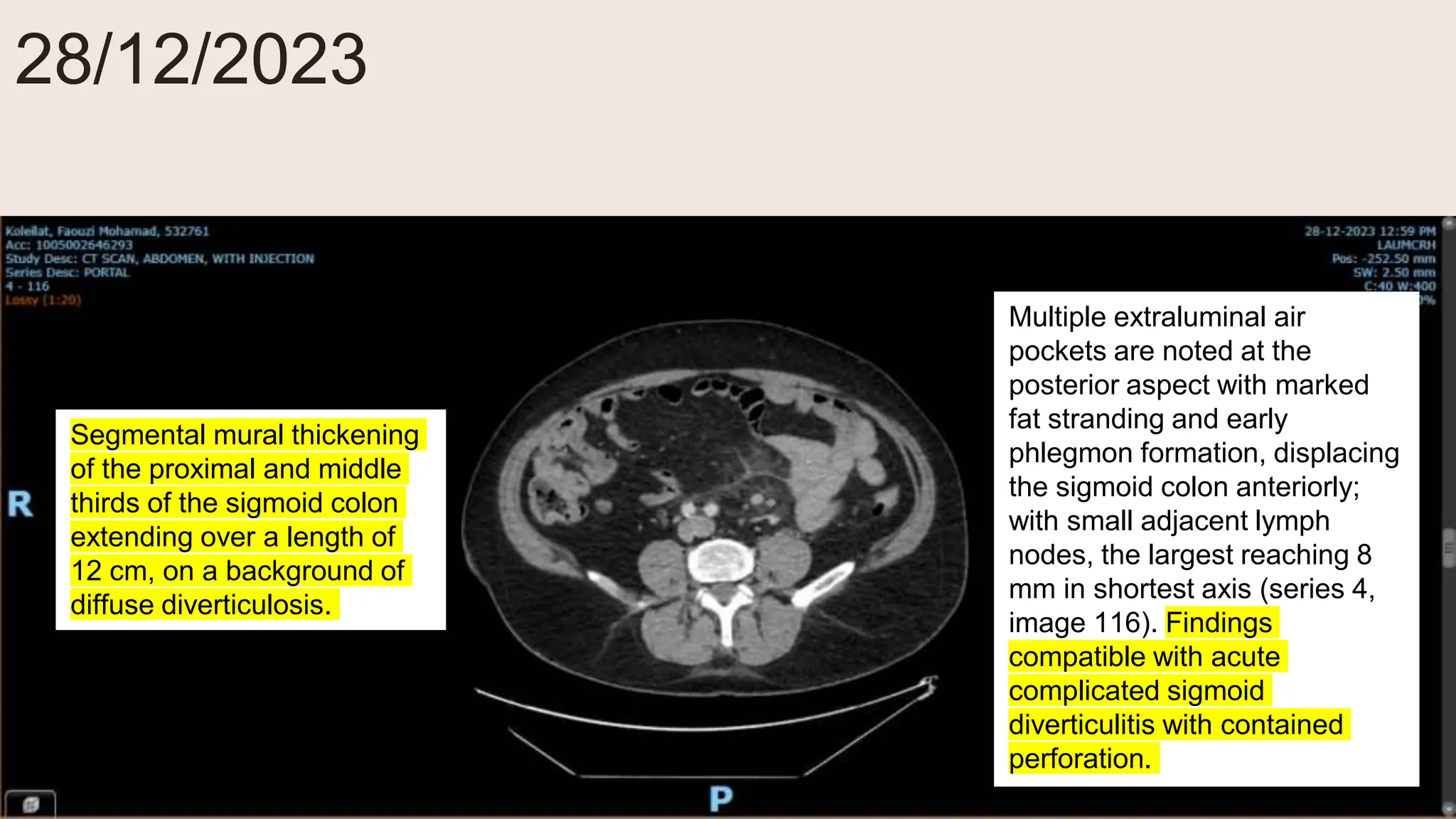
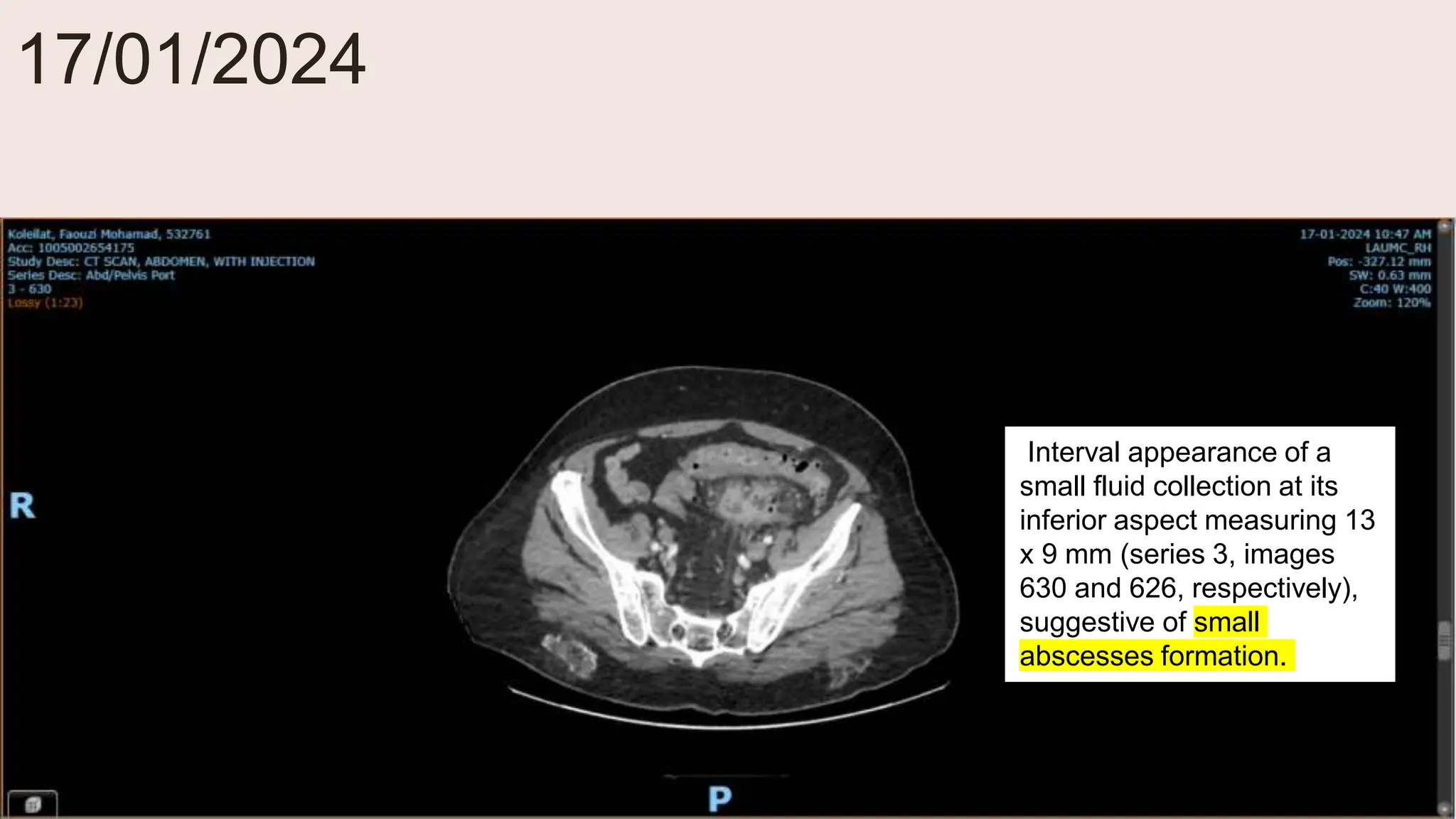
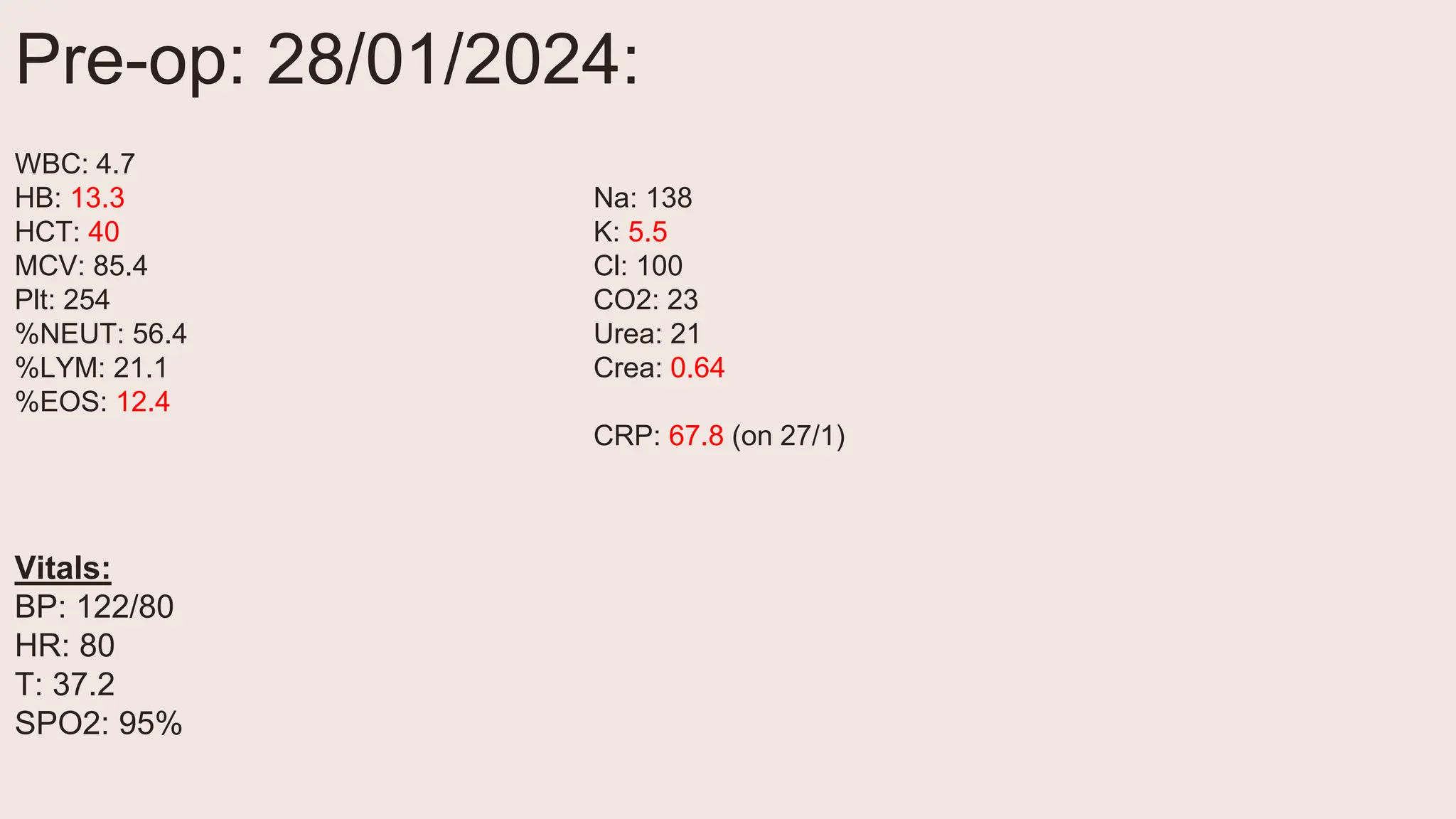
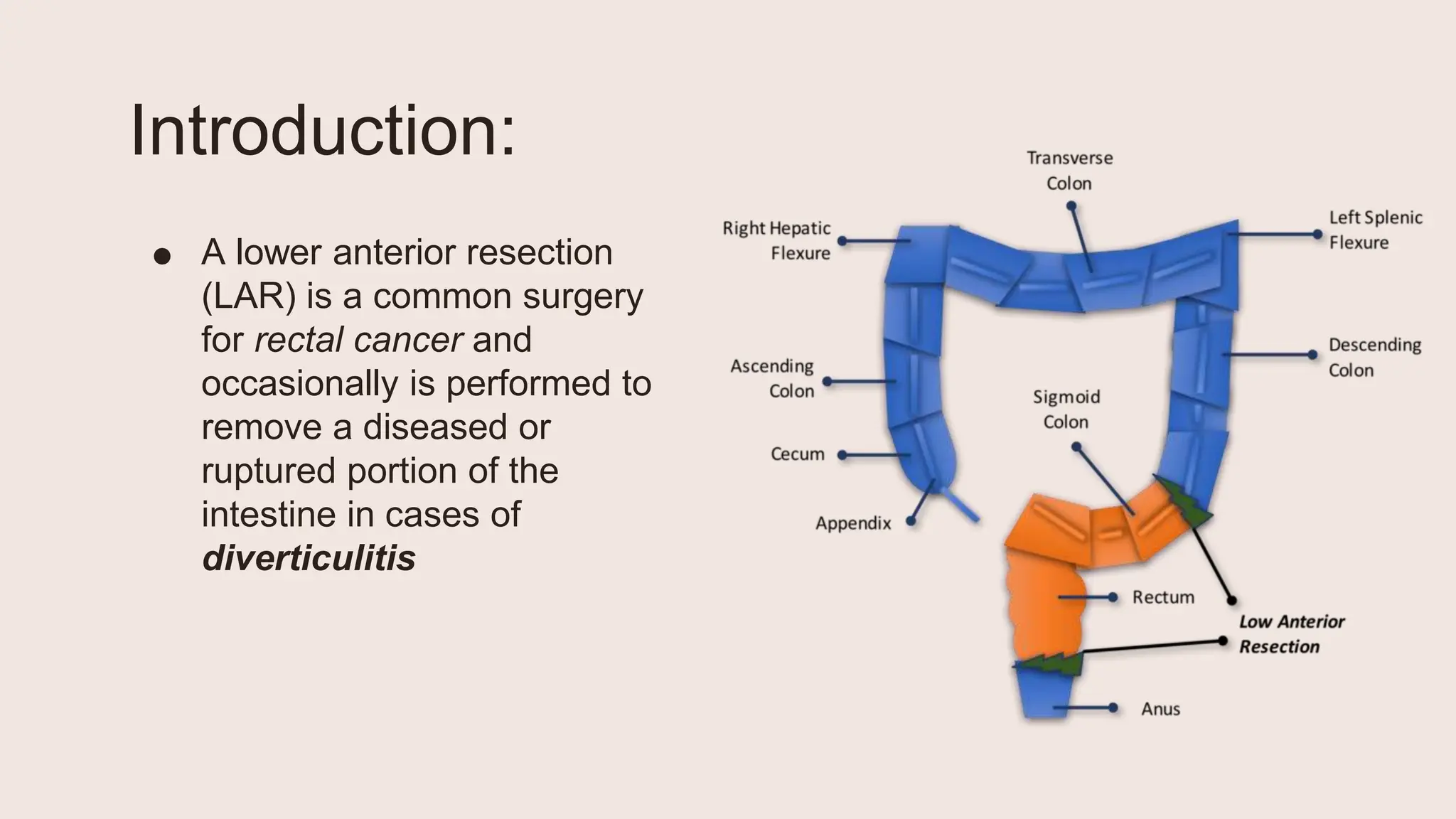
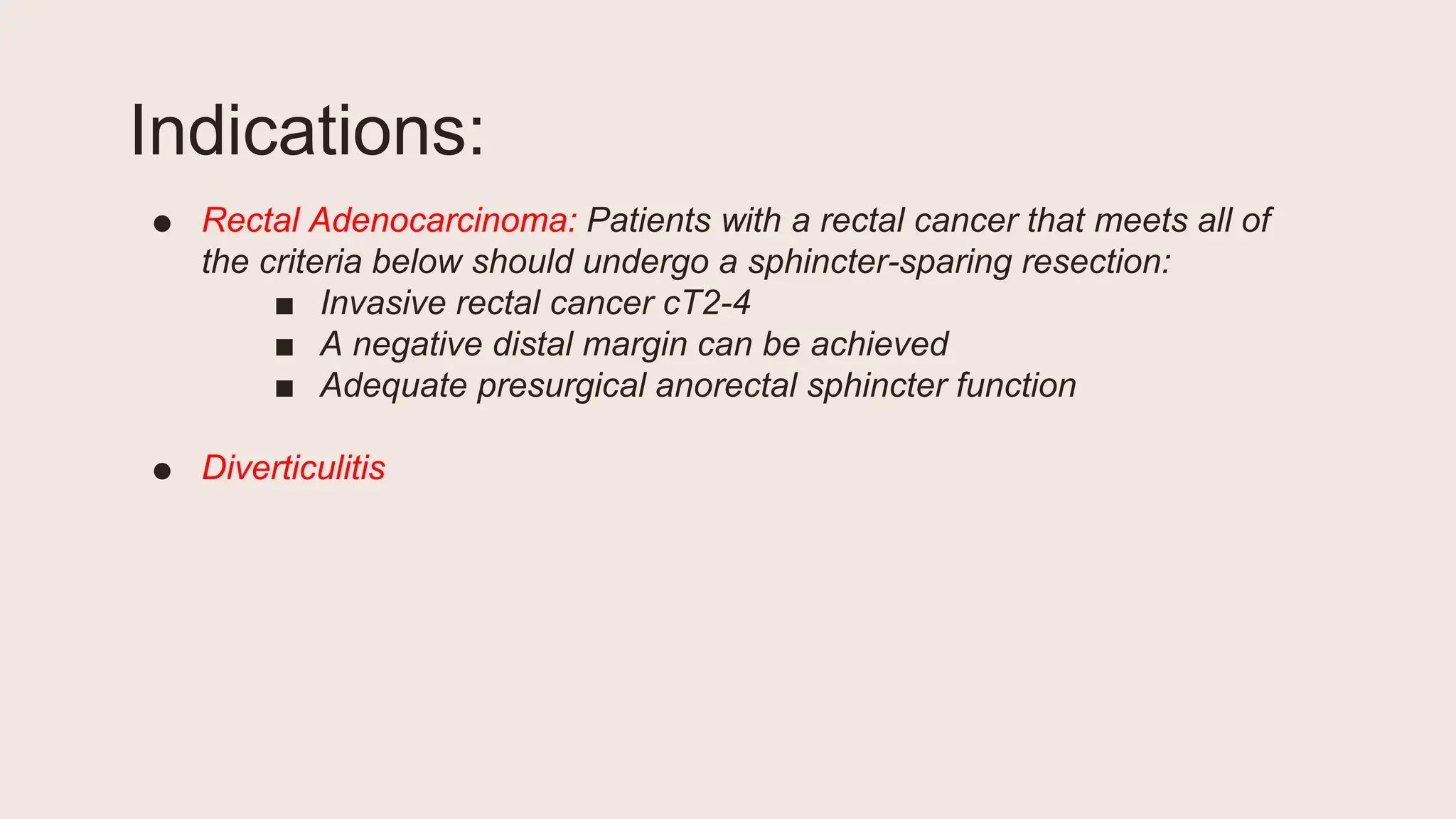
1) A 60-year-old male presented with severe abdominal pain and was found to have complicated diverticulitis of the sigmoid colon with contained perforation.
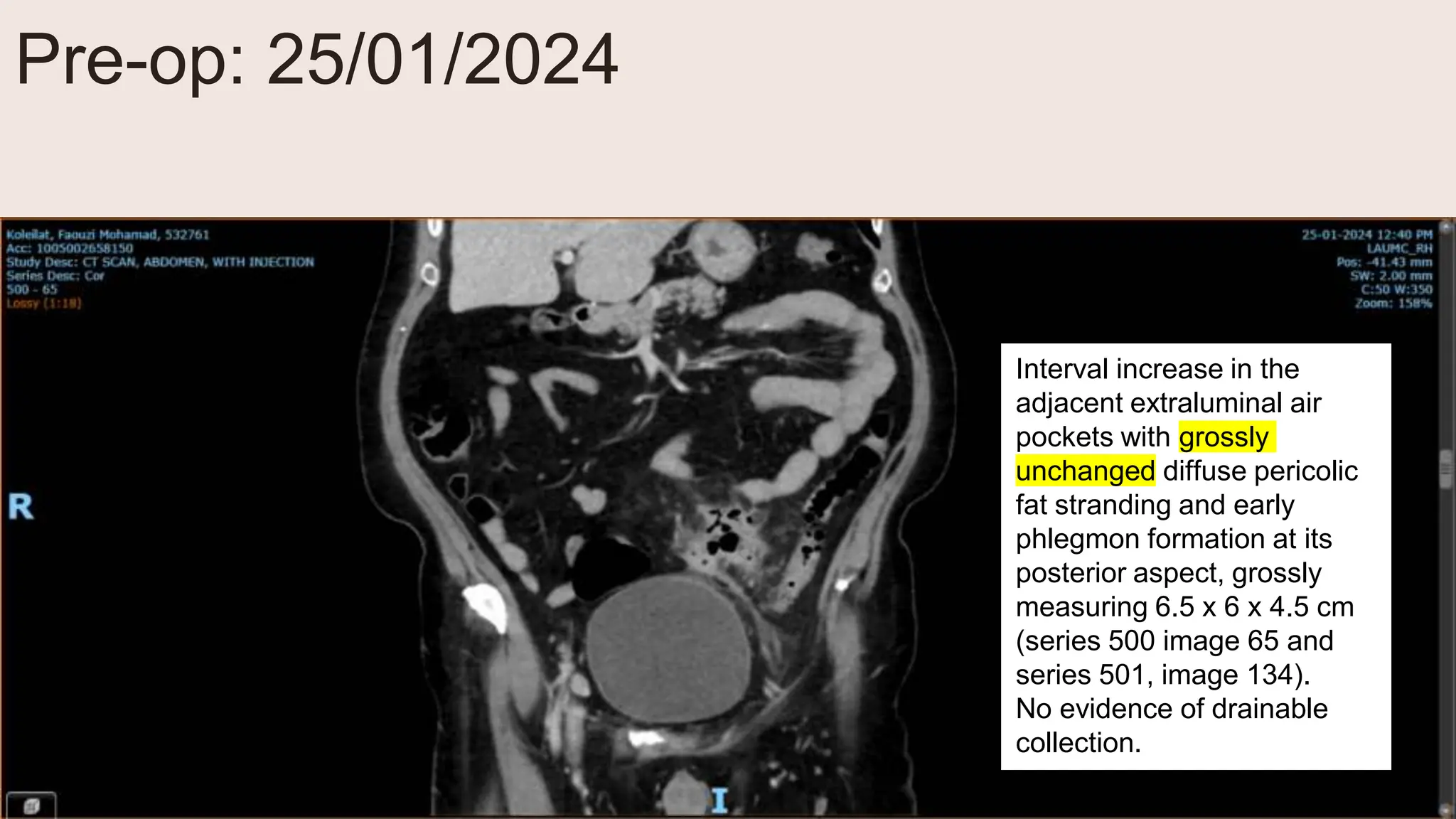
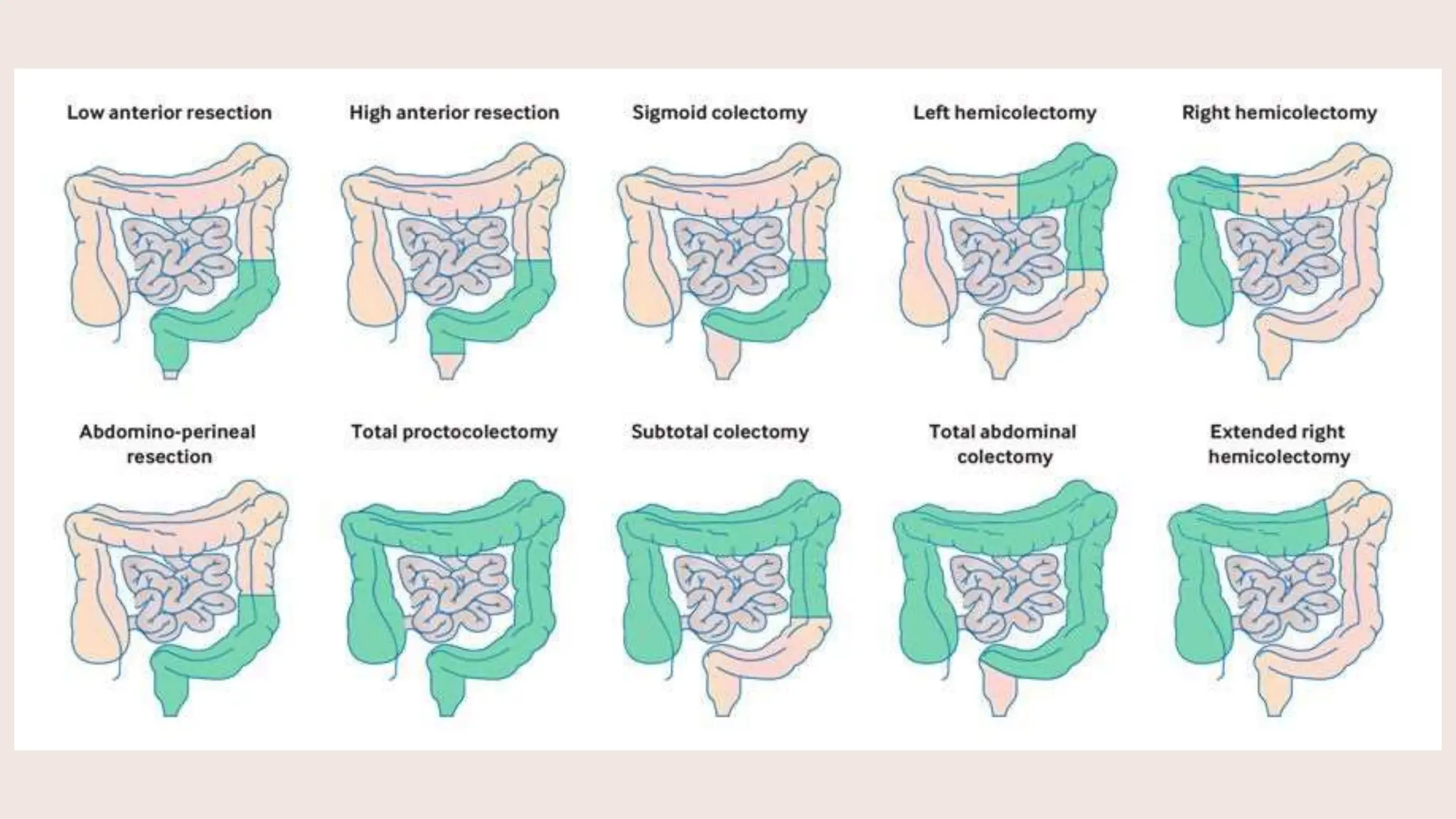
2) He underwent a laparoscopic low anterior resection to remove the diseased portion of colon.
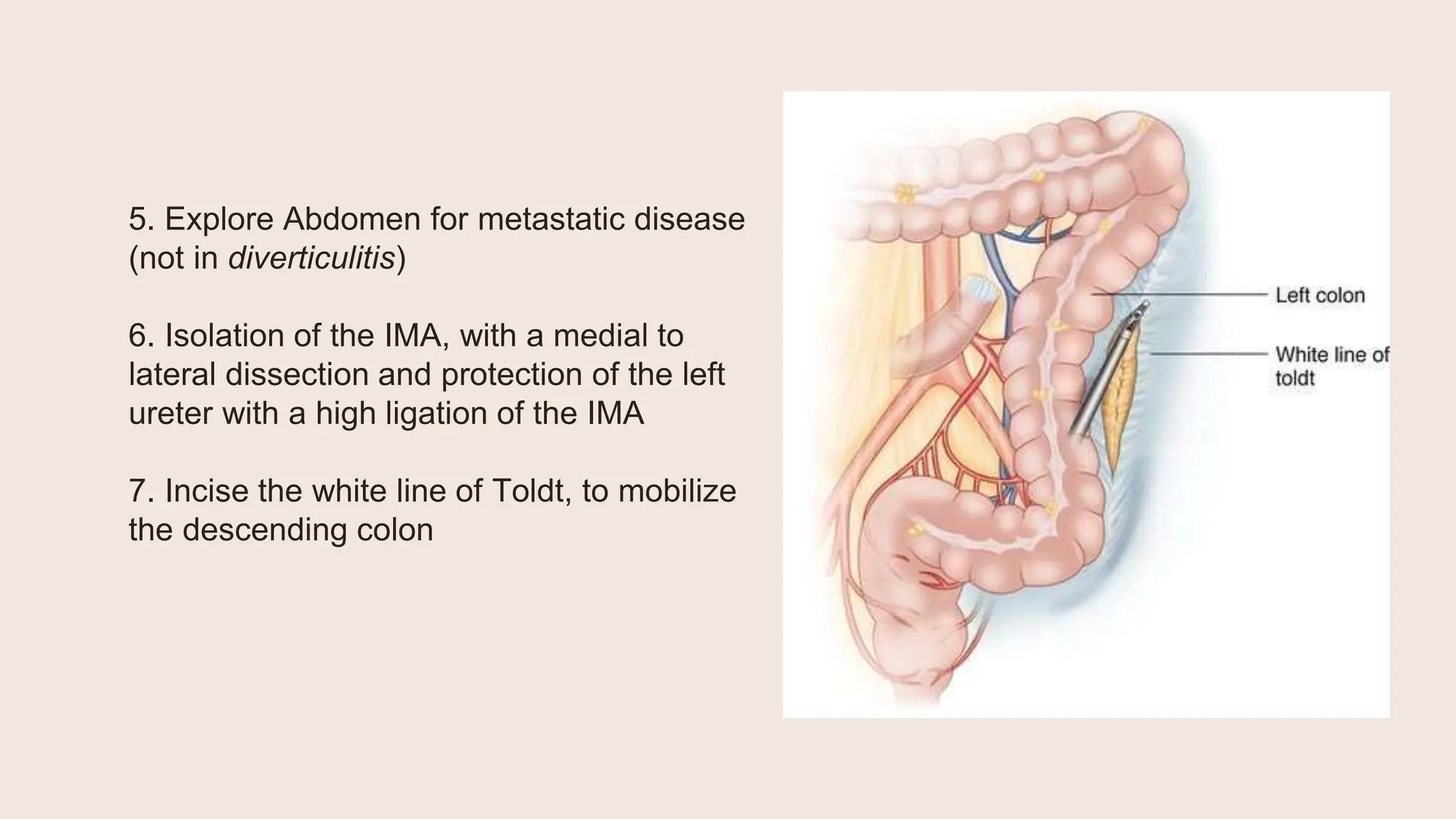
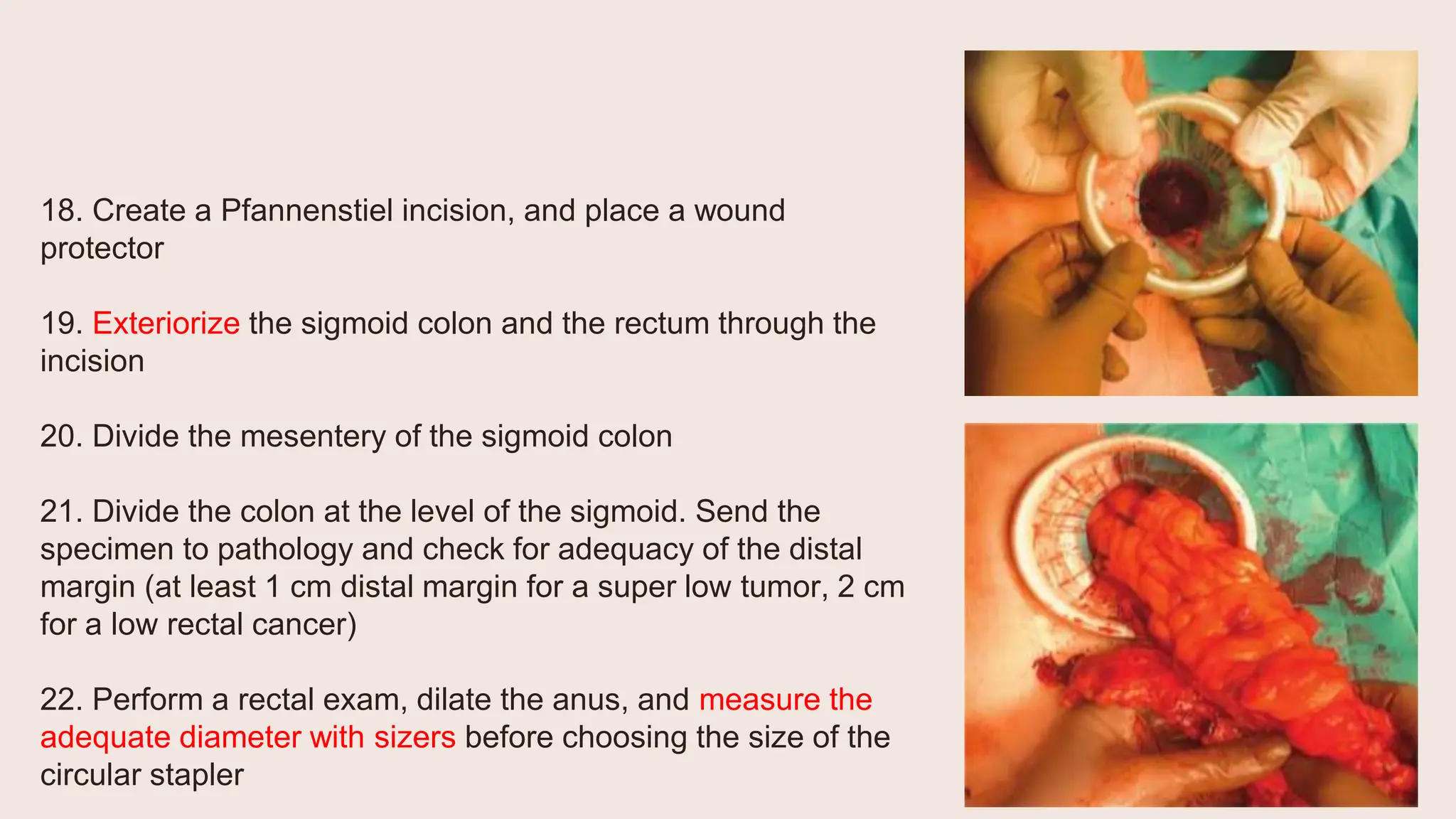
3) Key steps of the laparoscopic low anterior resection included mobilization of the descending colon and sigmoid mesocolon, ligation of the inferior mesenteric artery, dissection of the rectum, division of the rectum, creation of an end-to-end anastomosis, and possible creation of a temporary ileostomy.