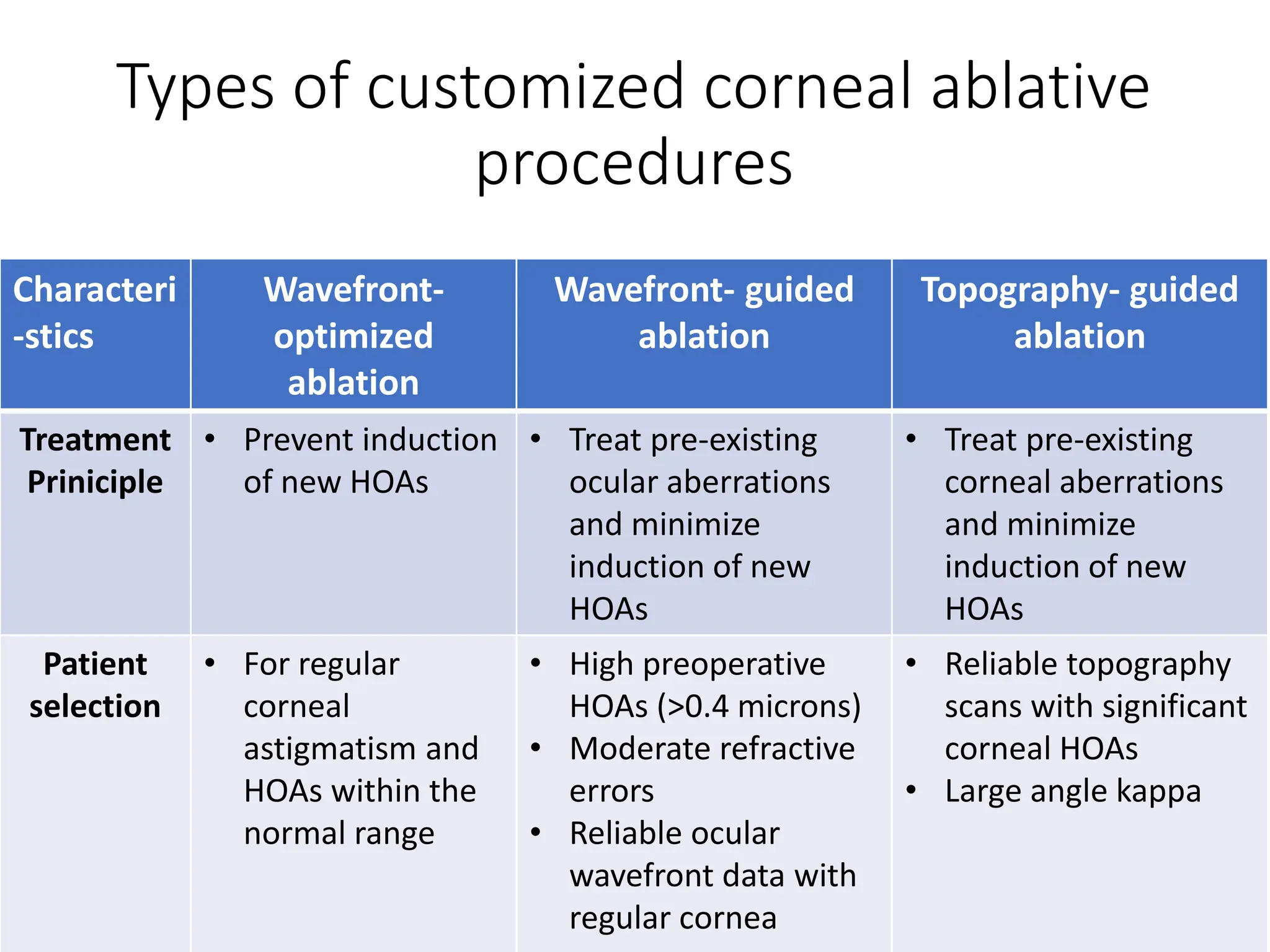
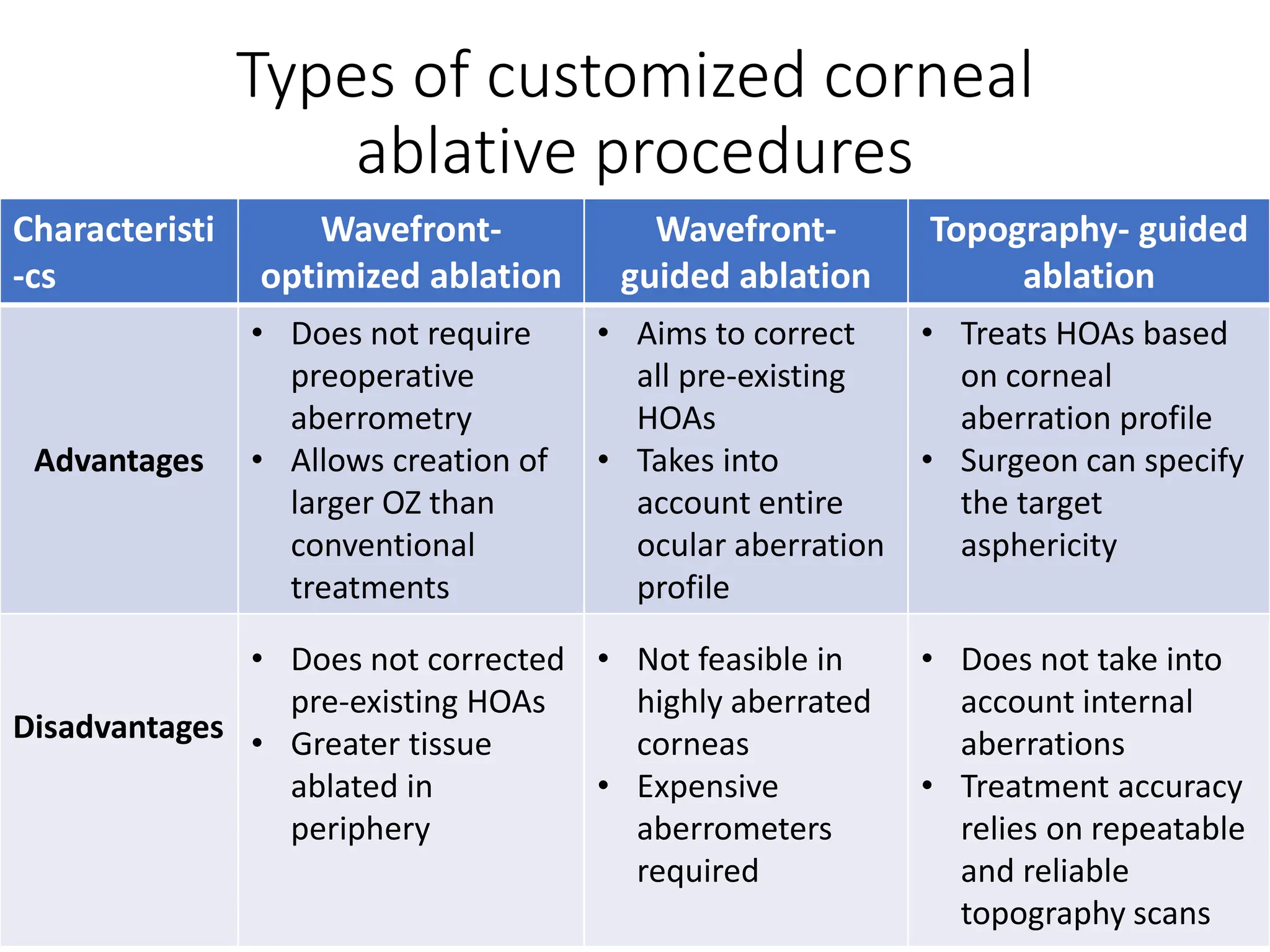
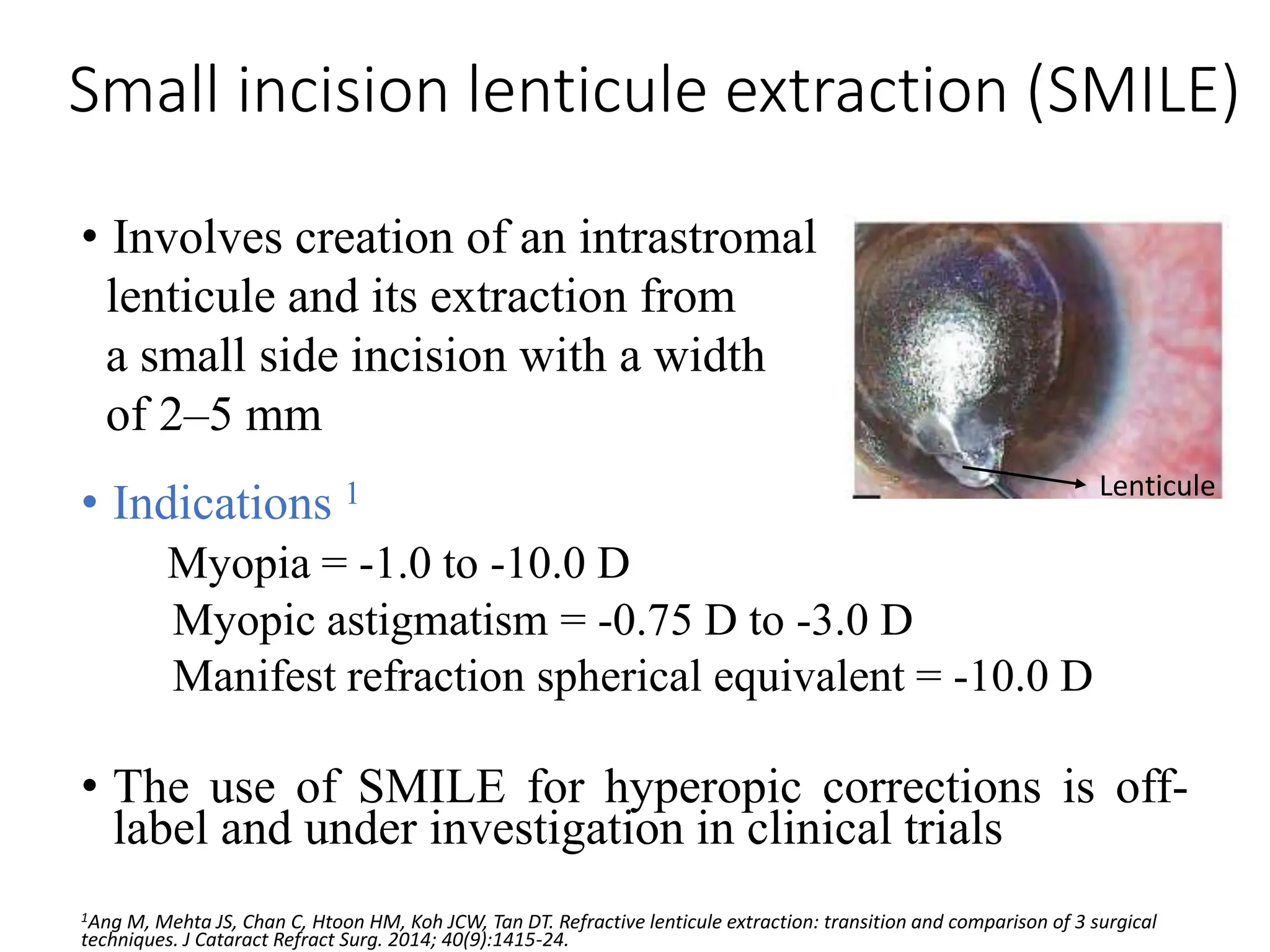
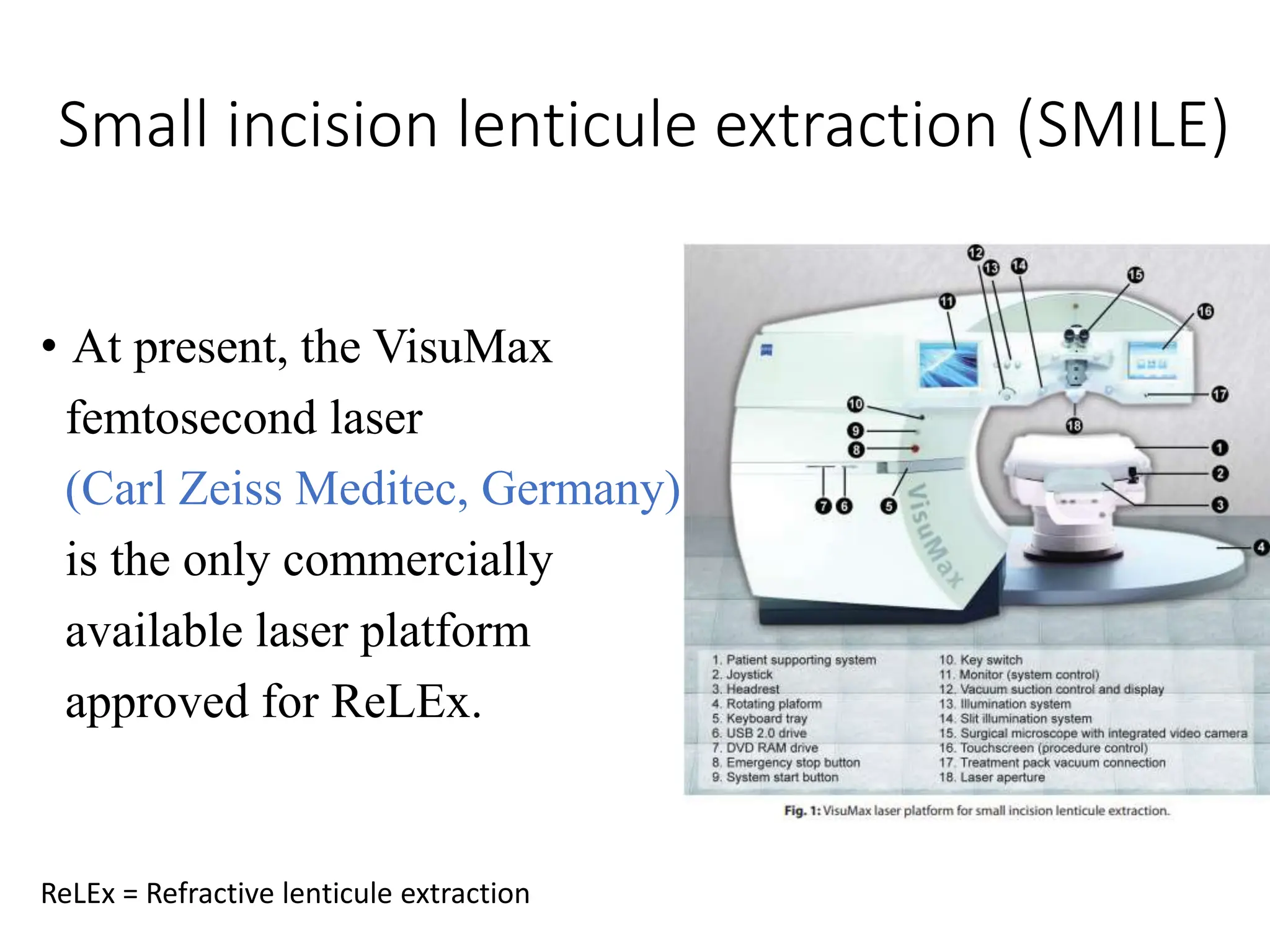
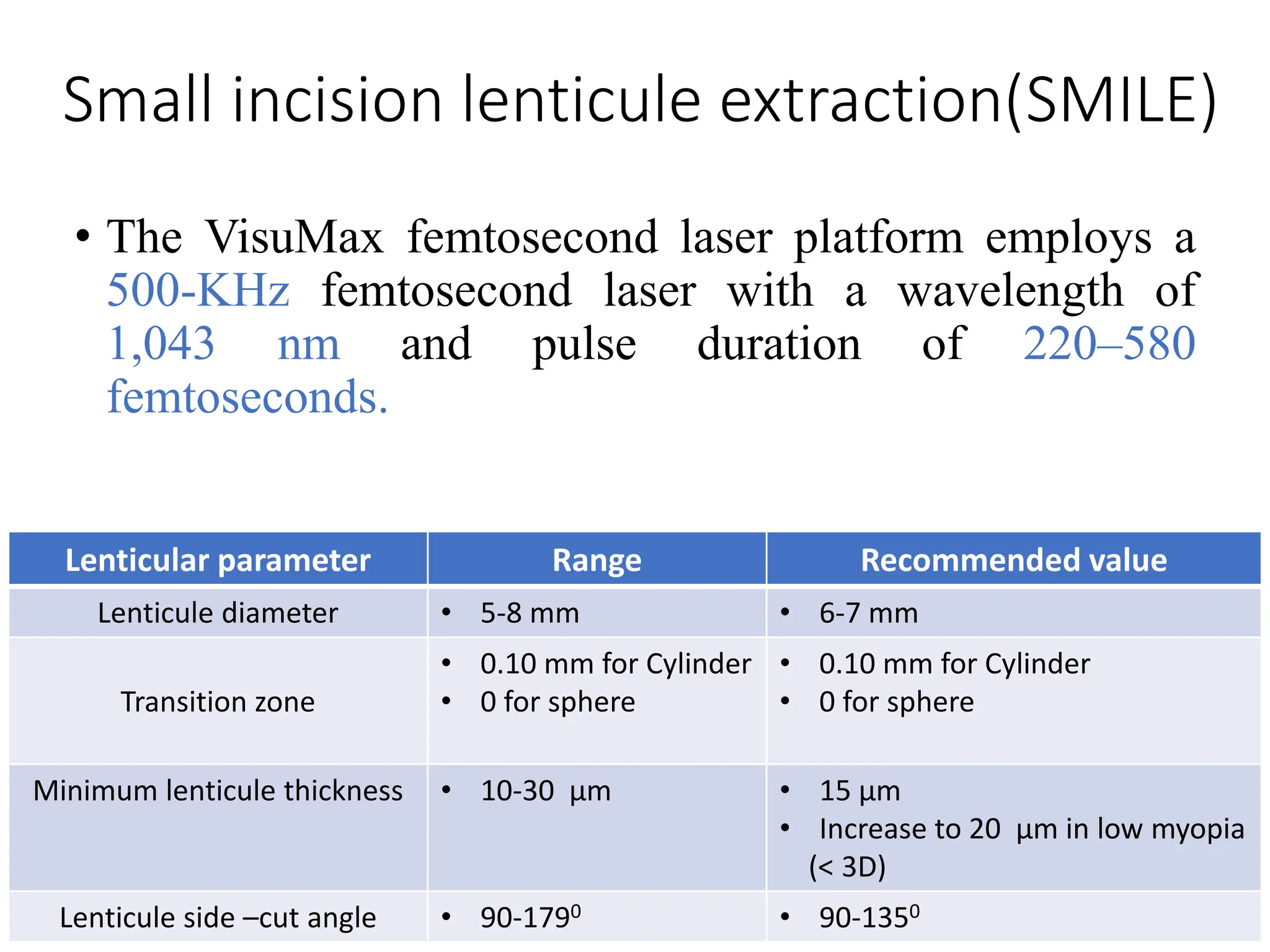
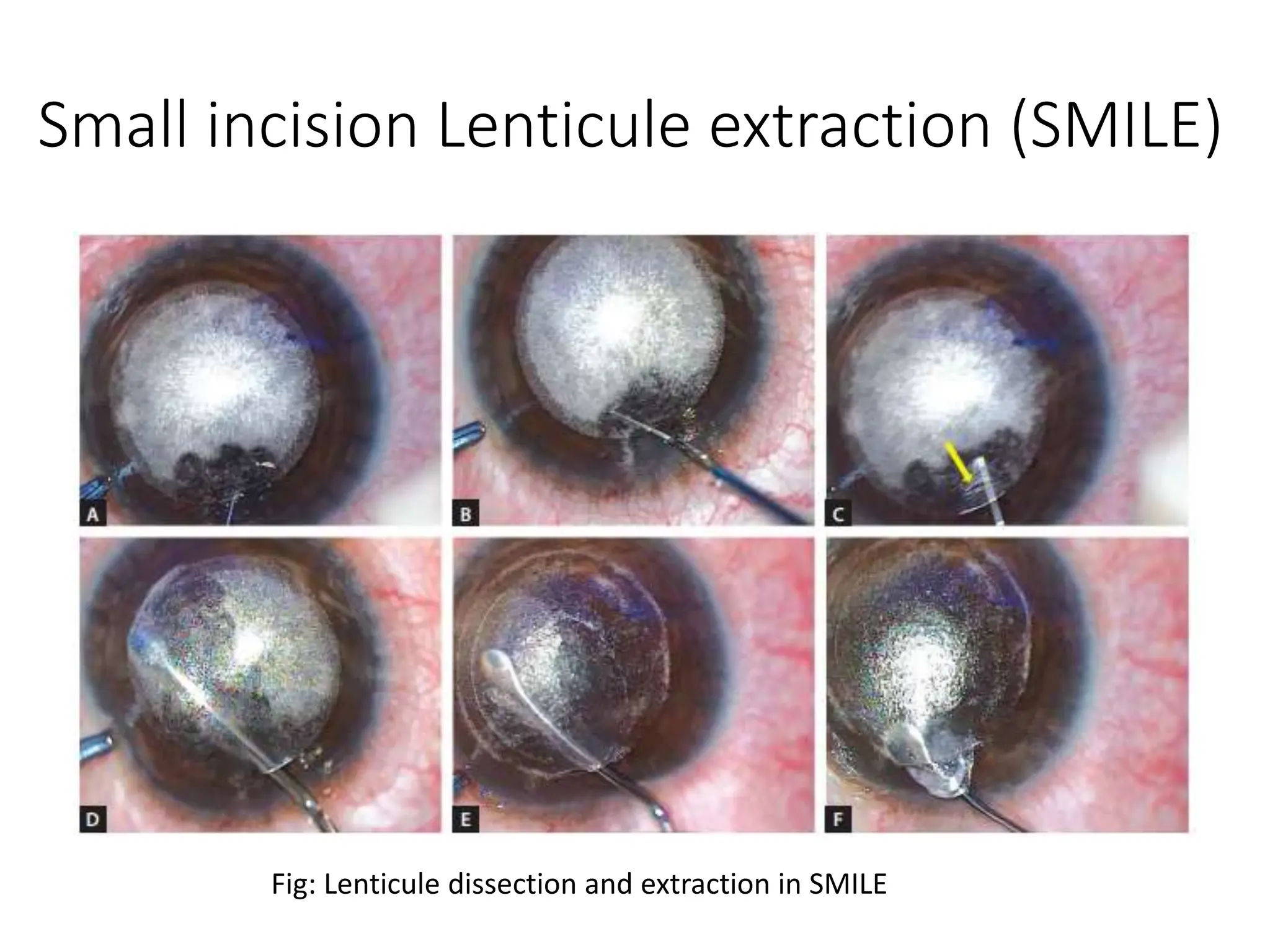
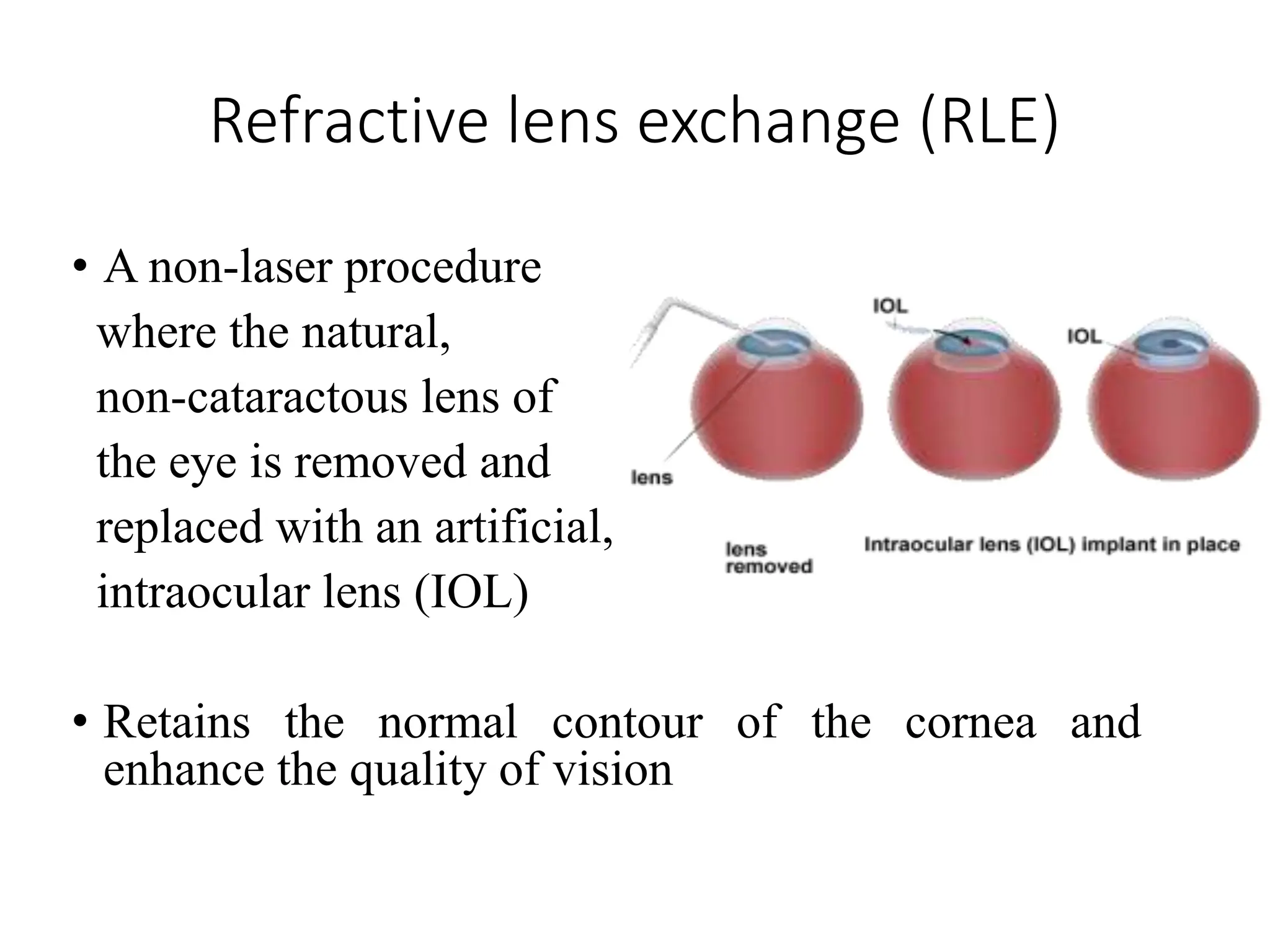
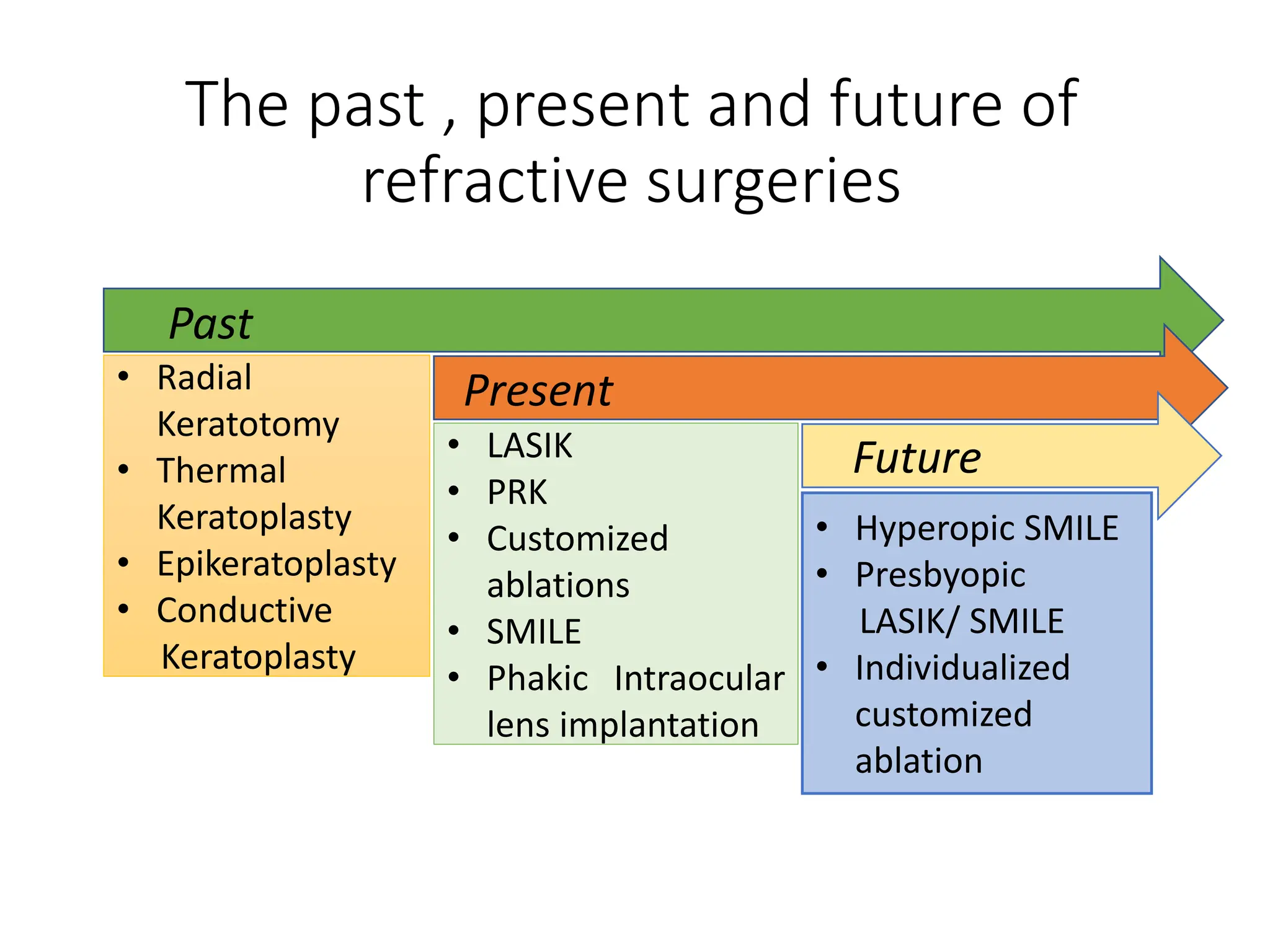
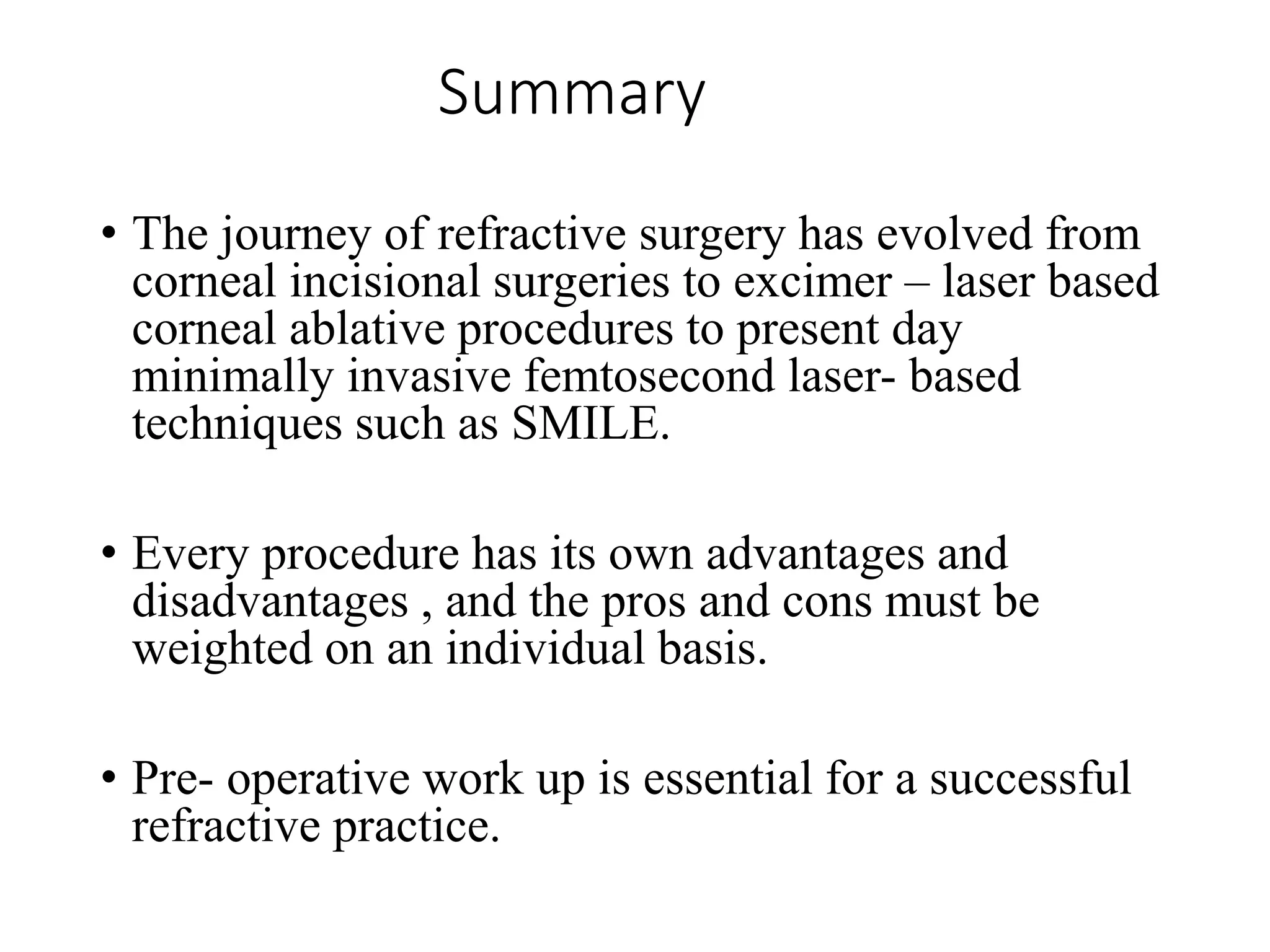
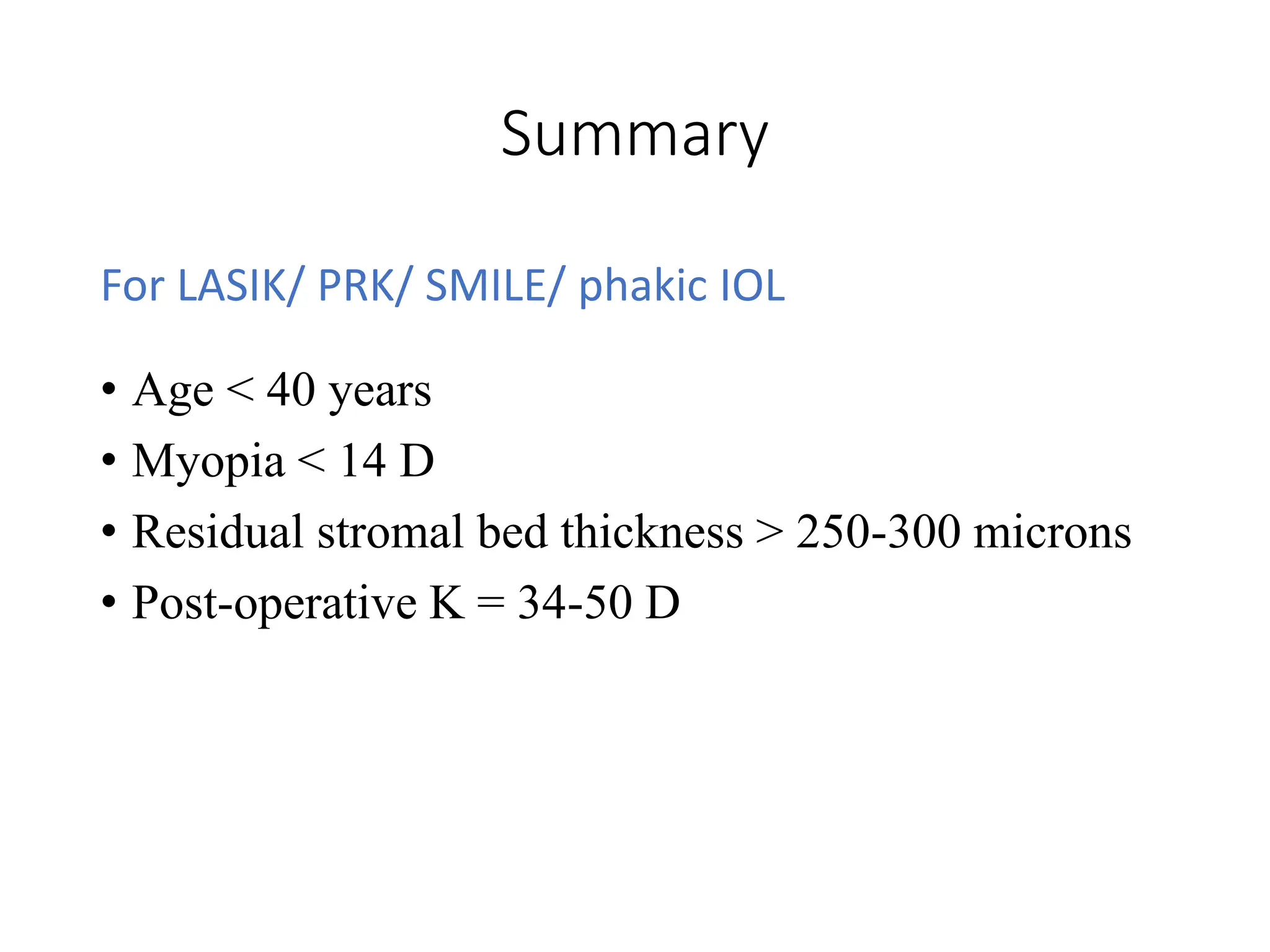
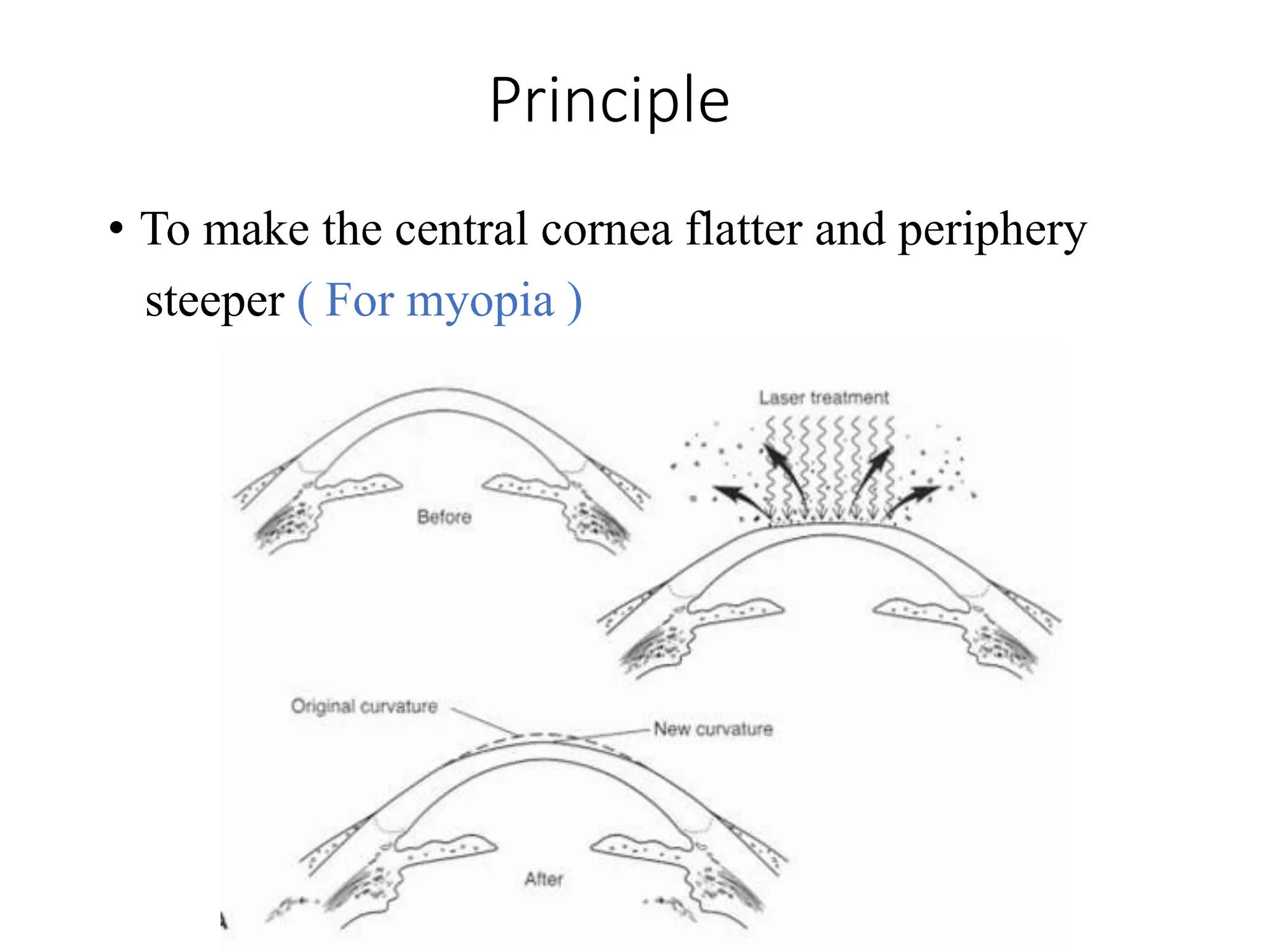
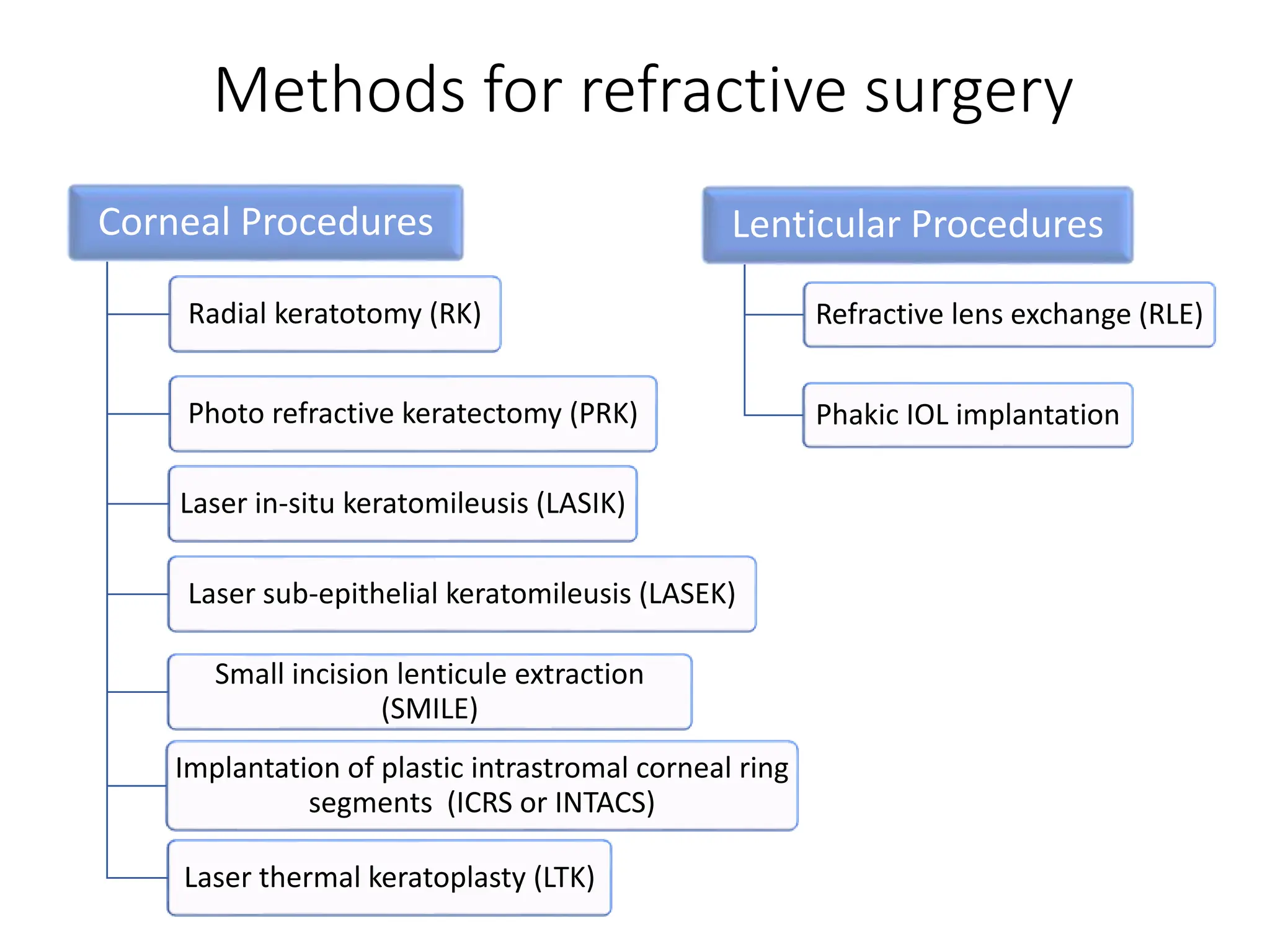
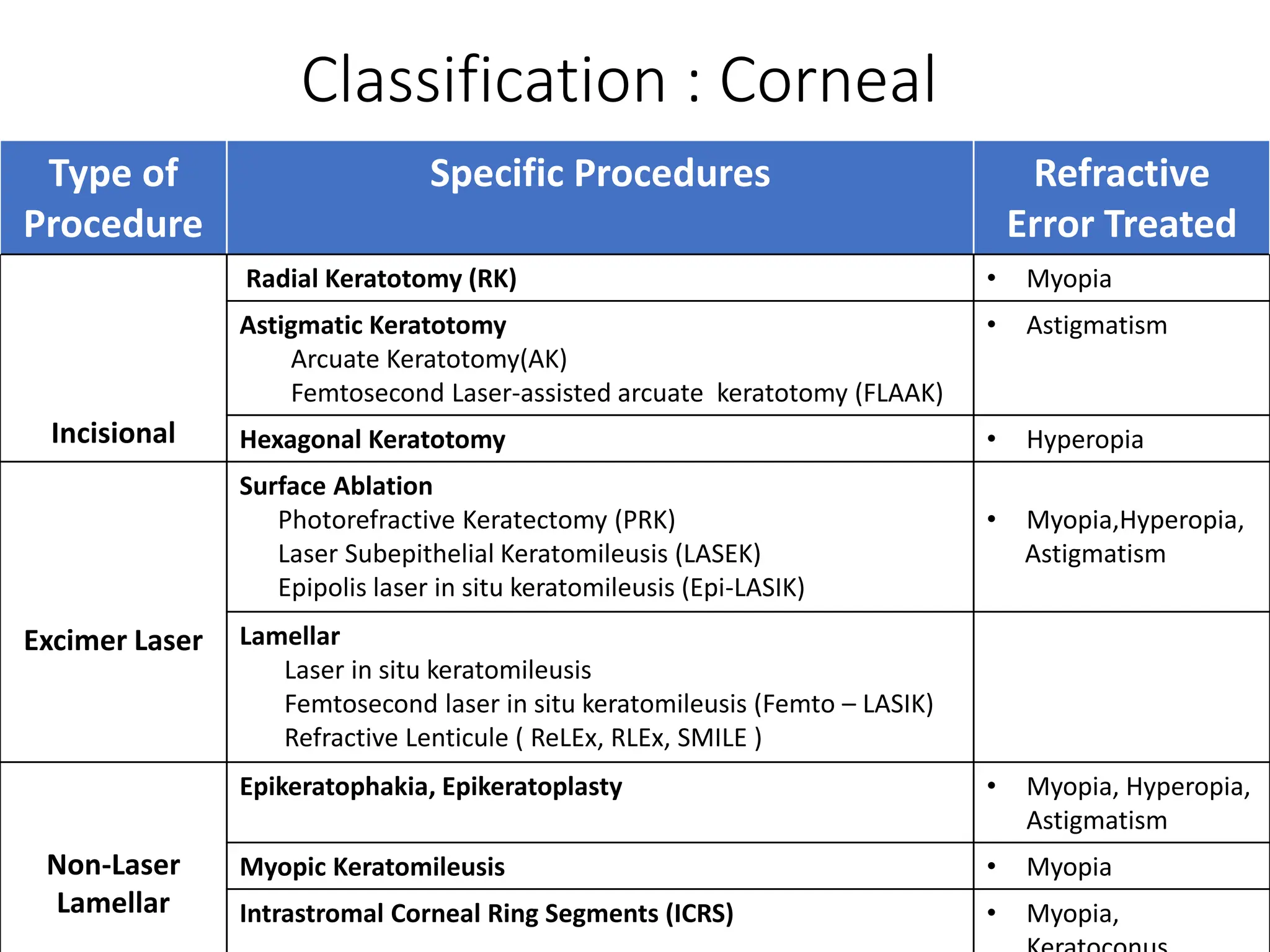
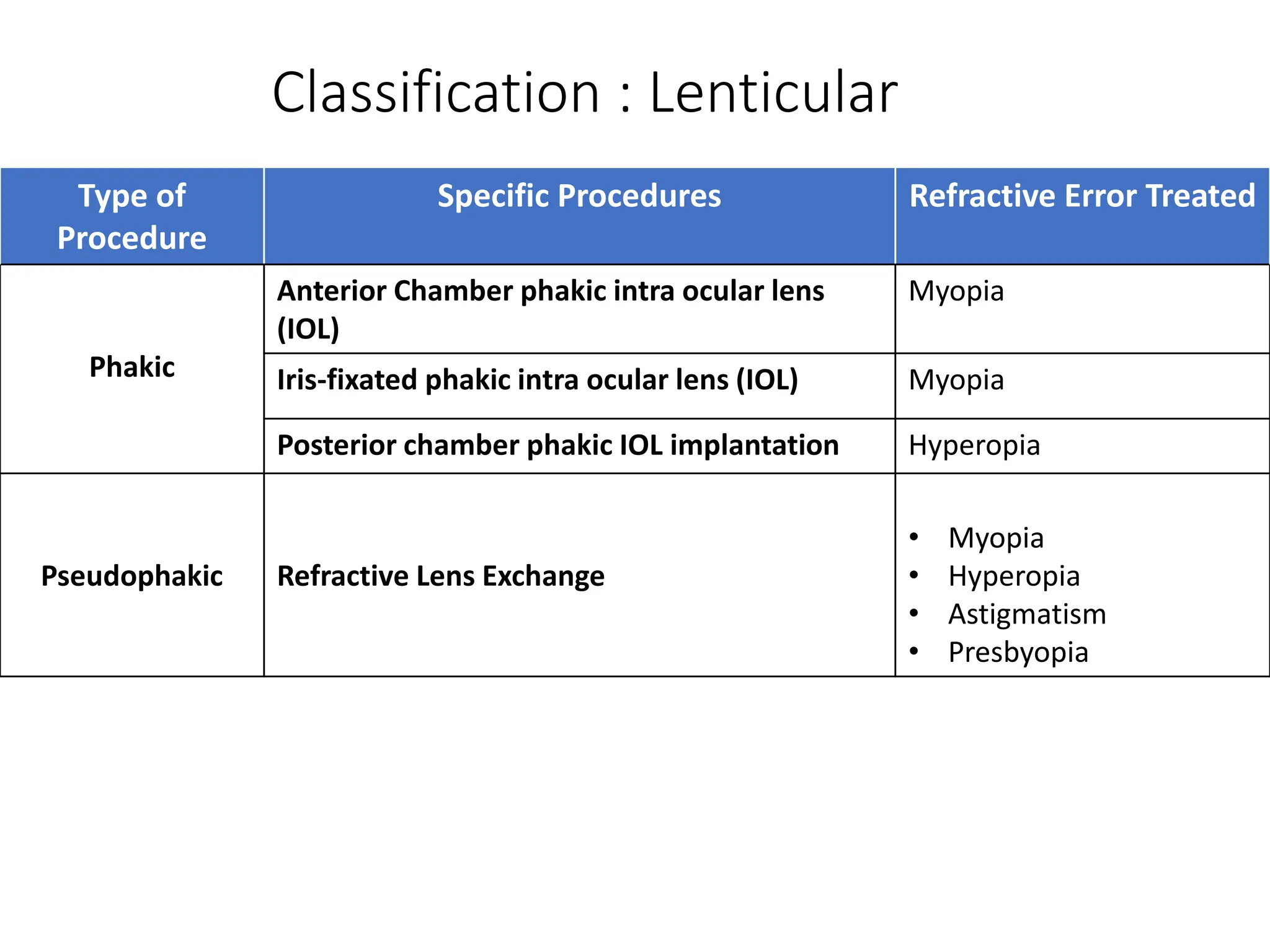
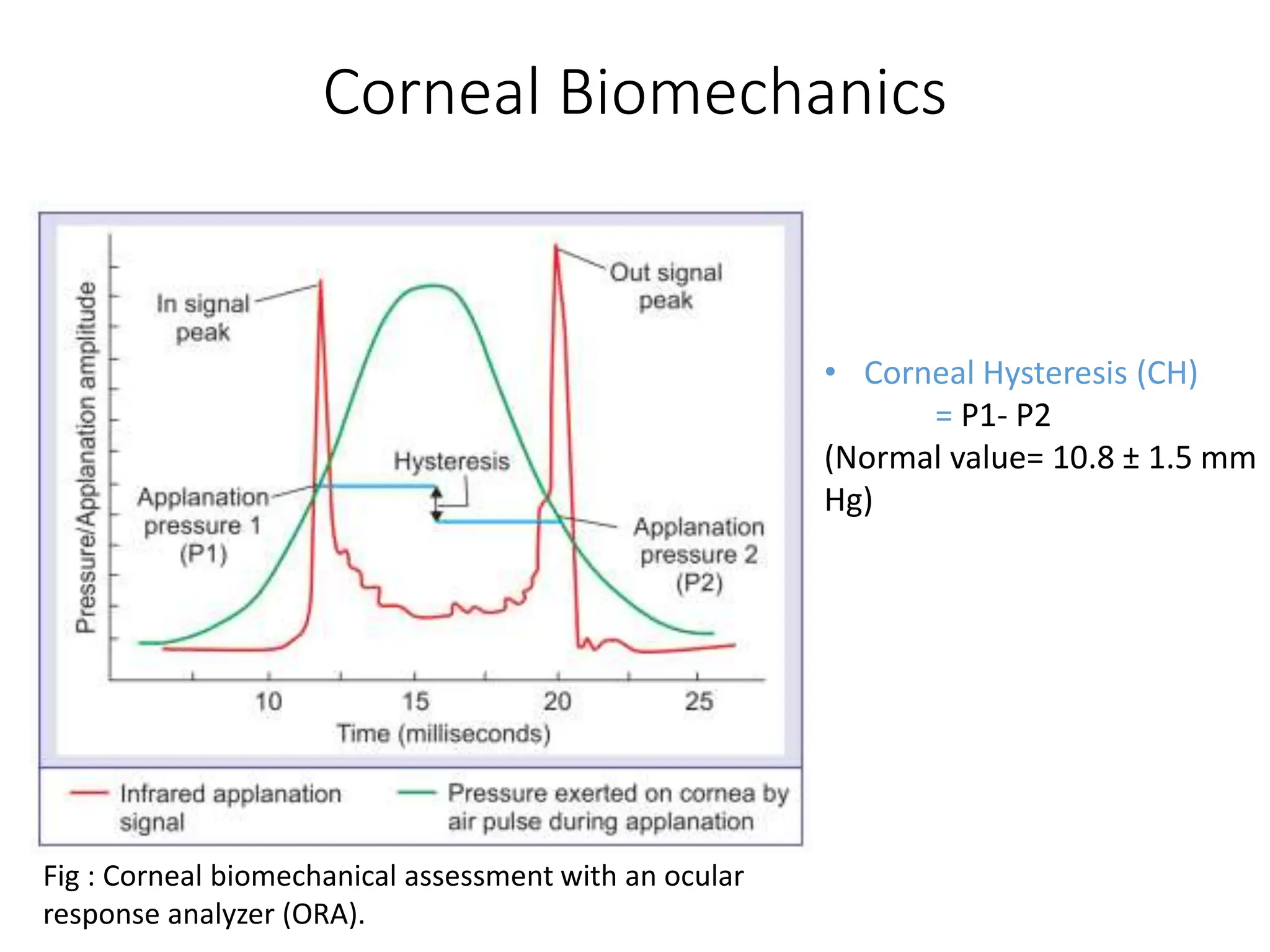
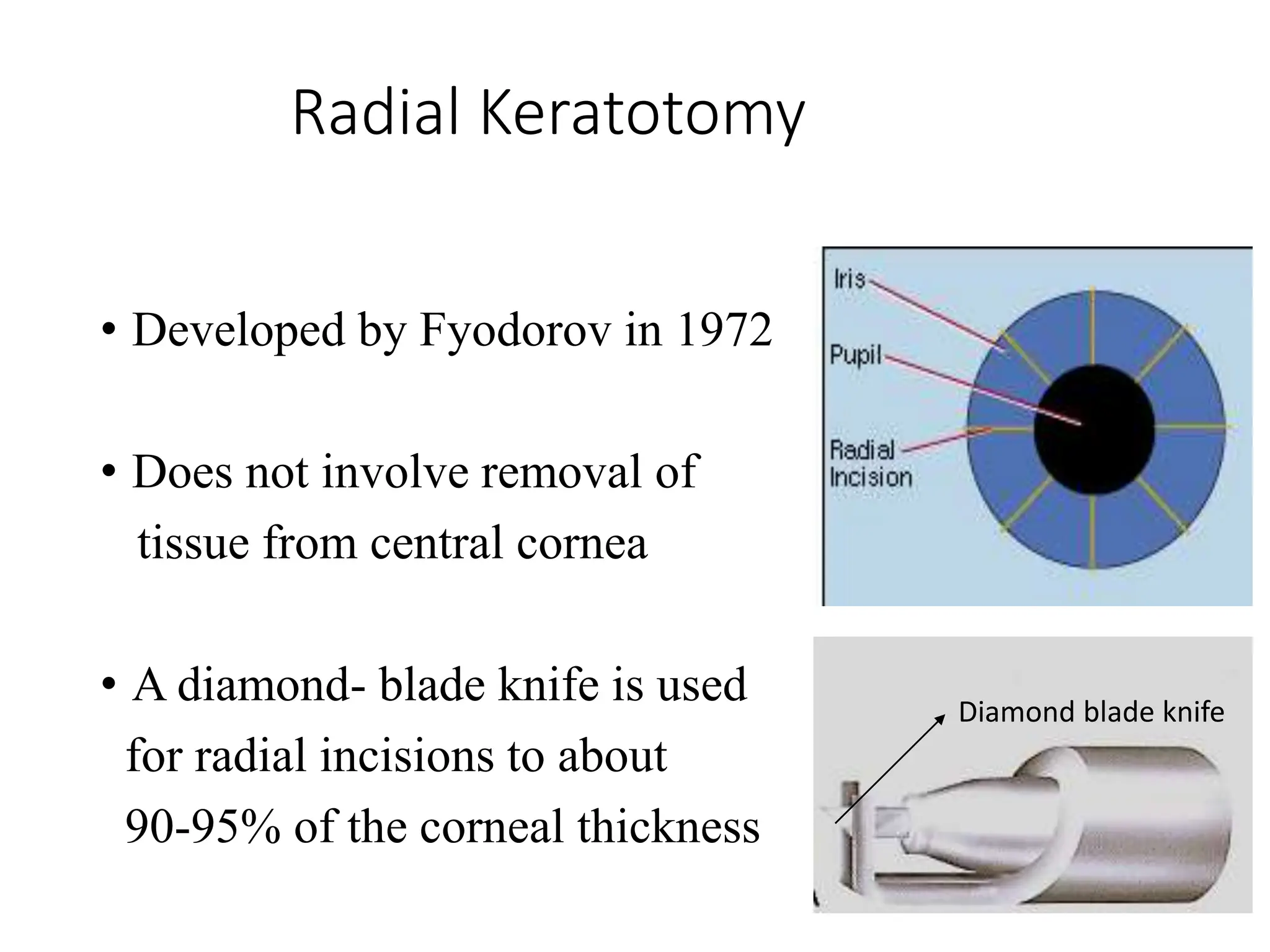
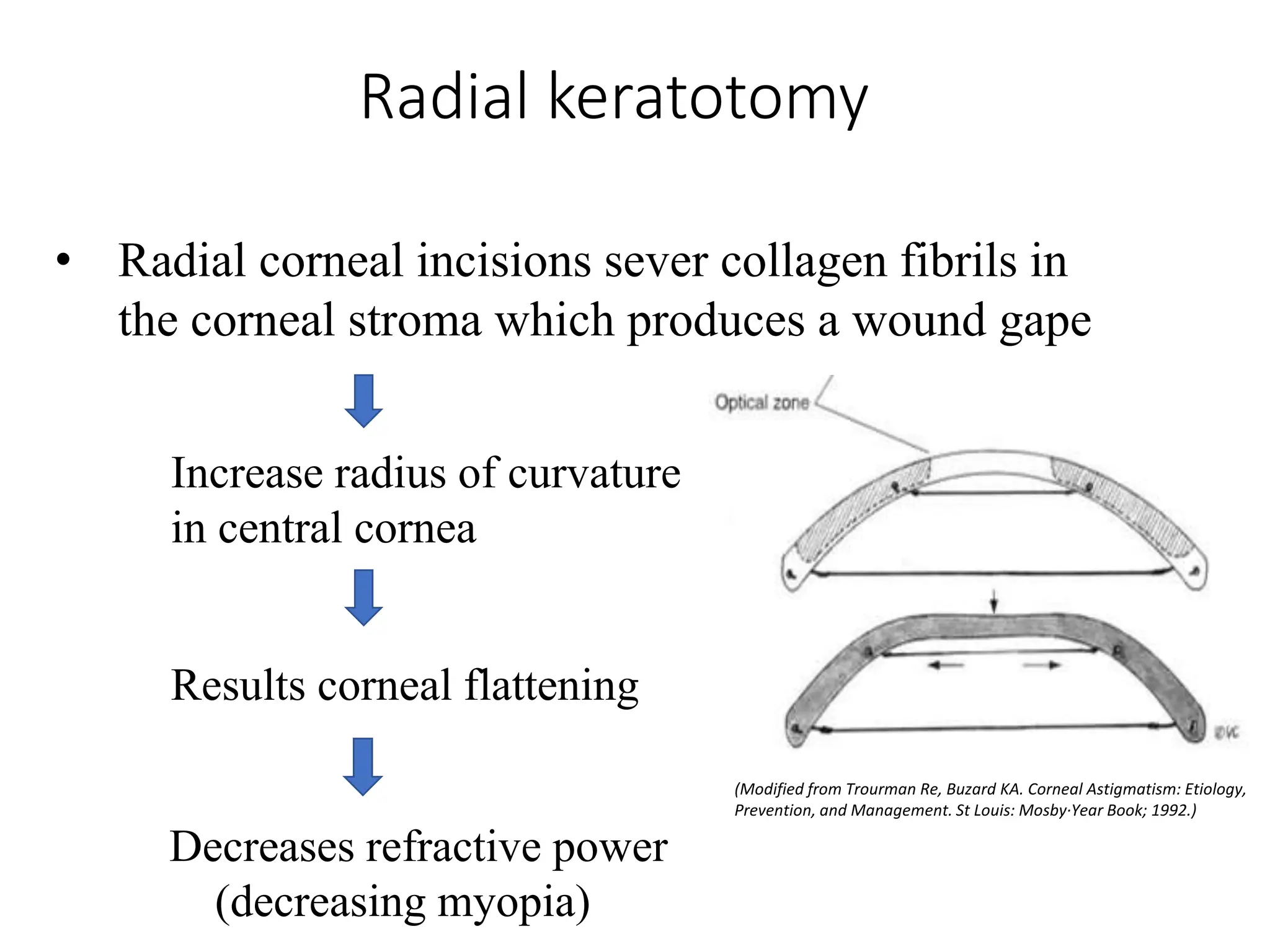
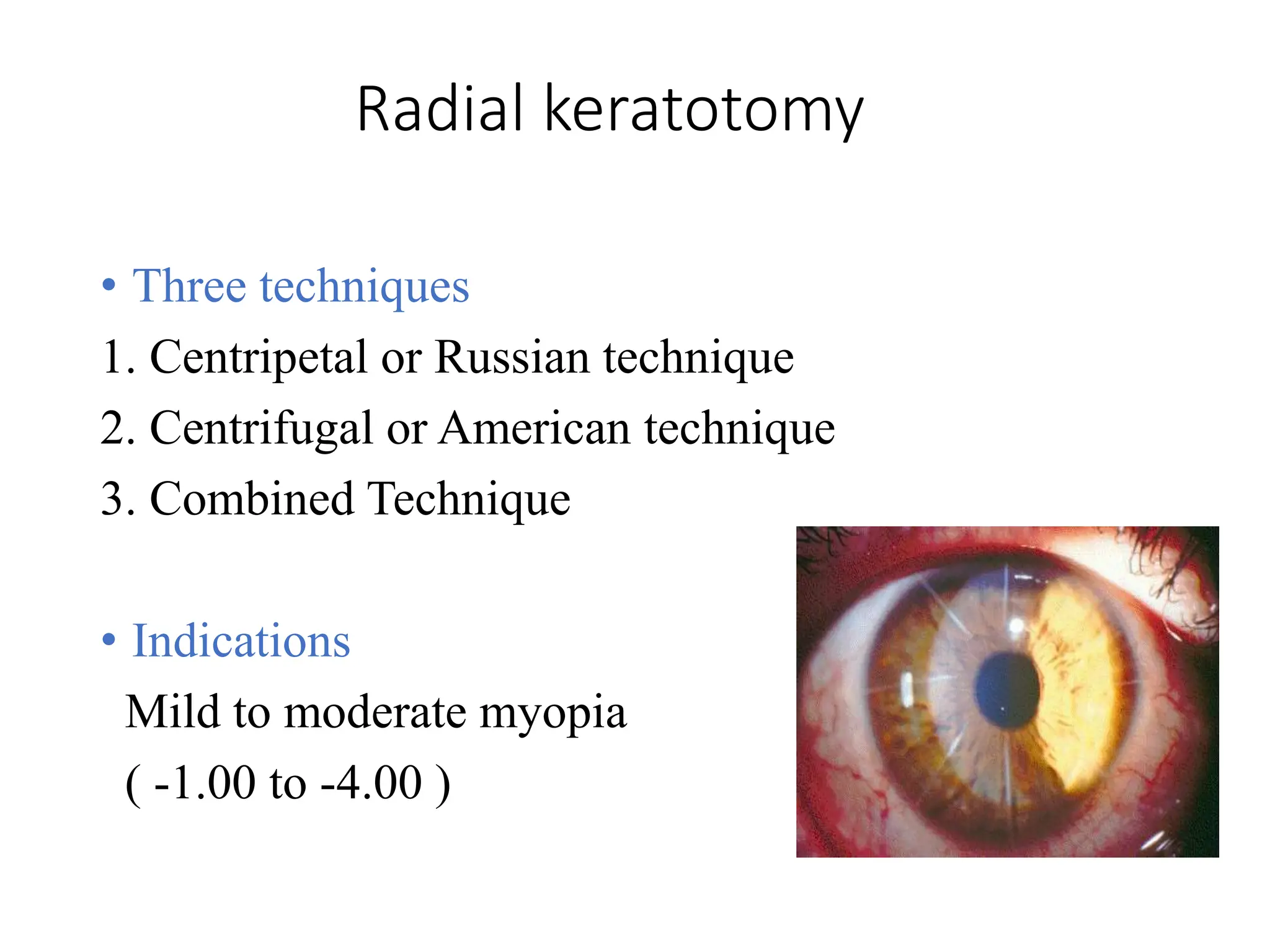
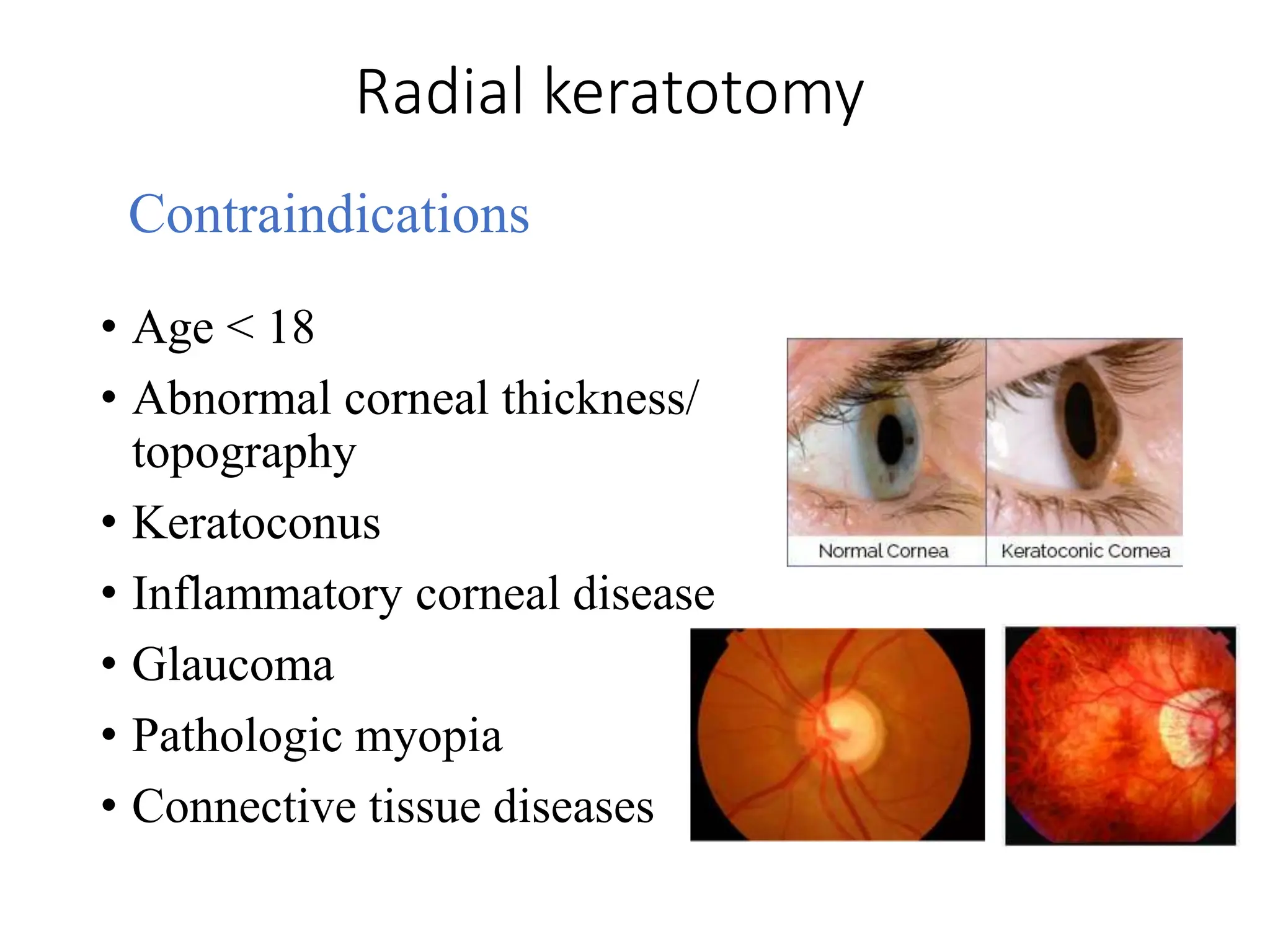
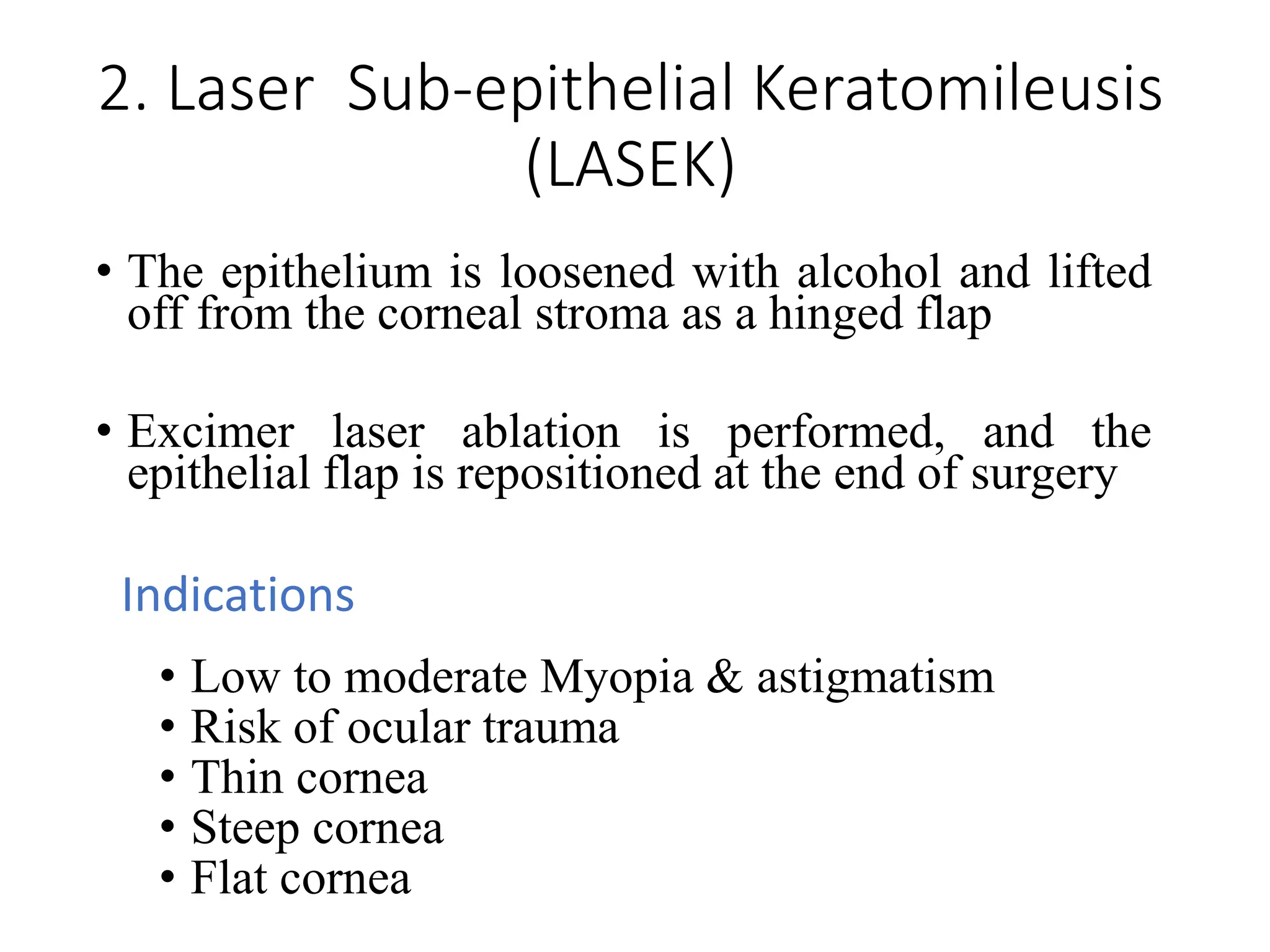
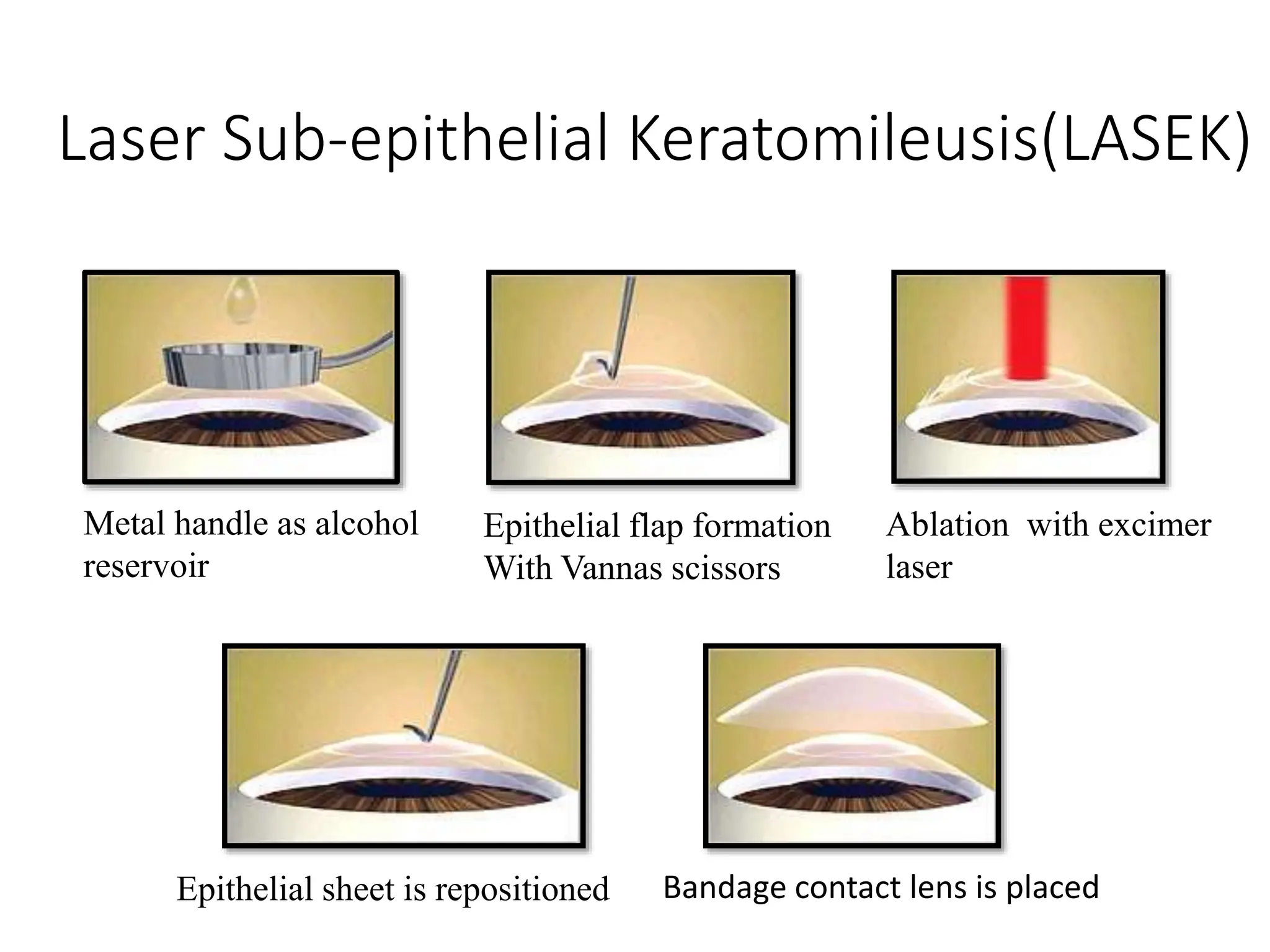
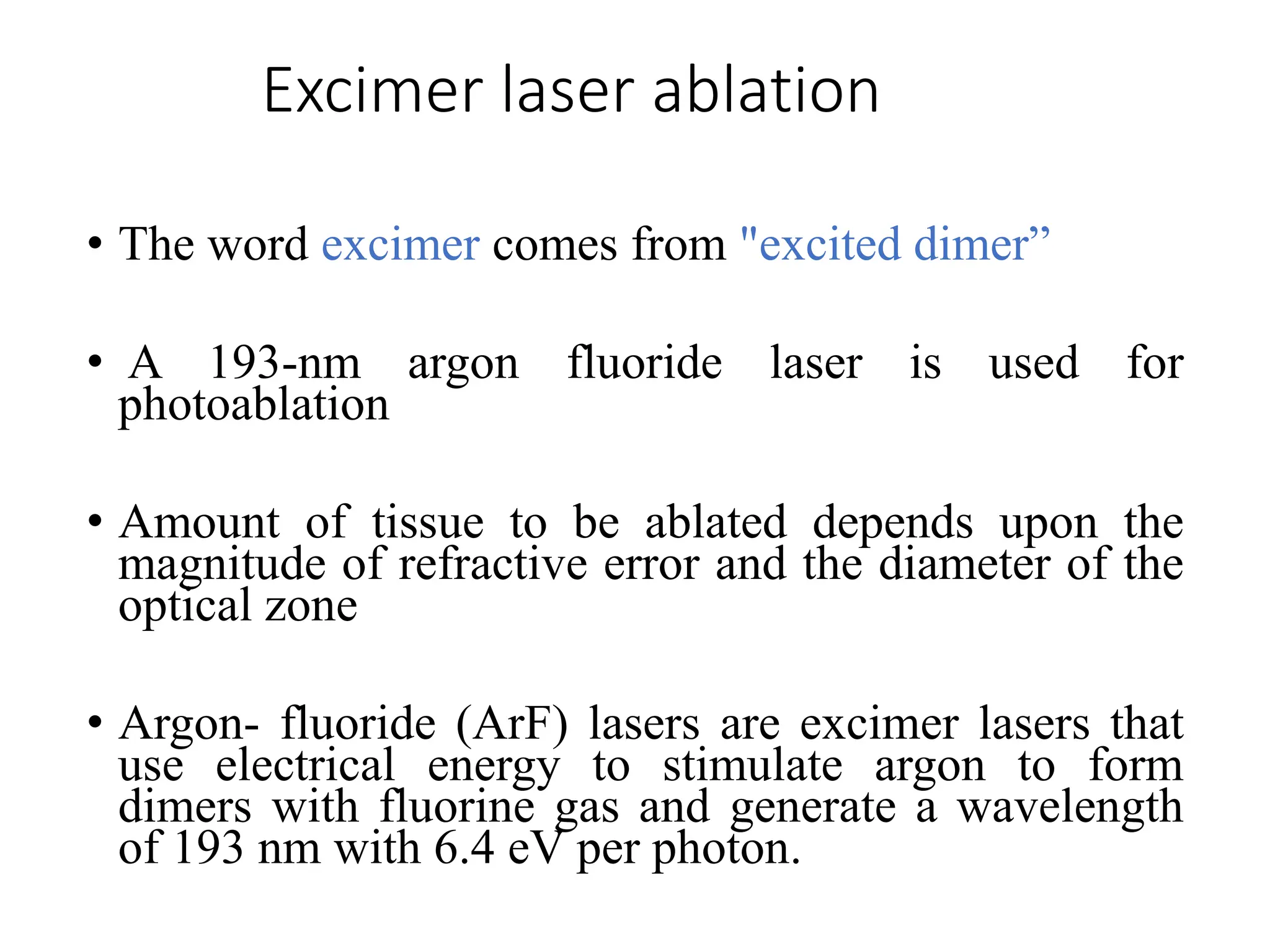
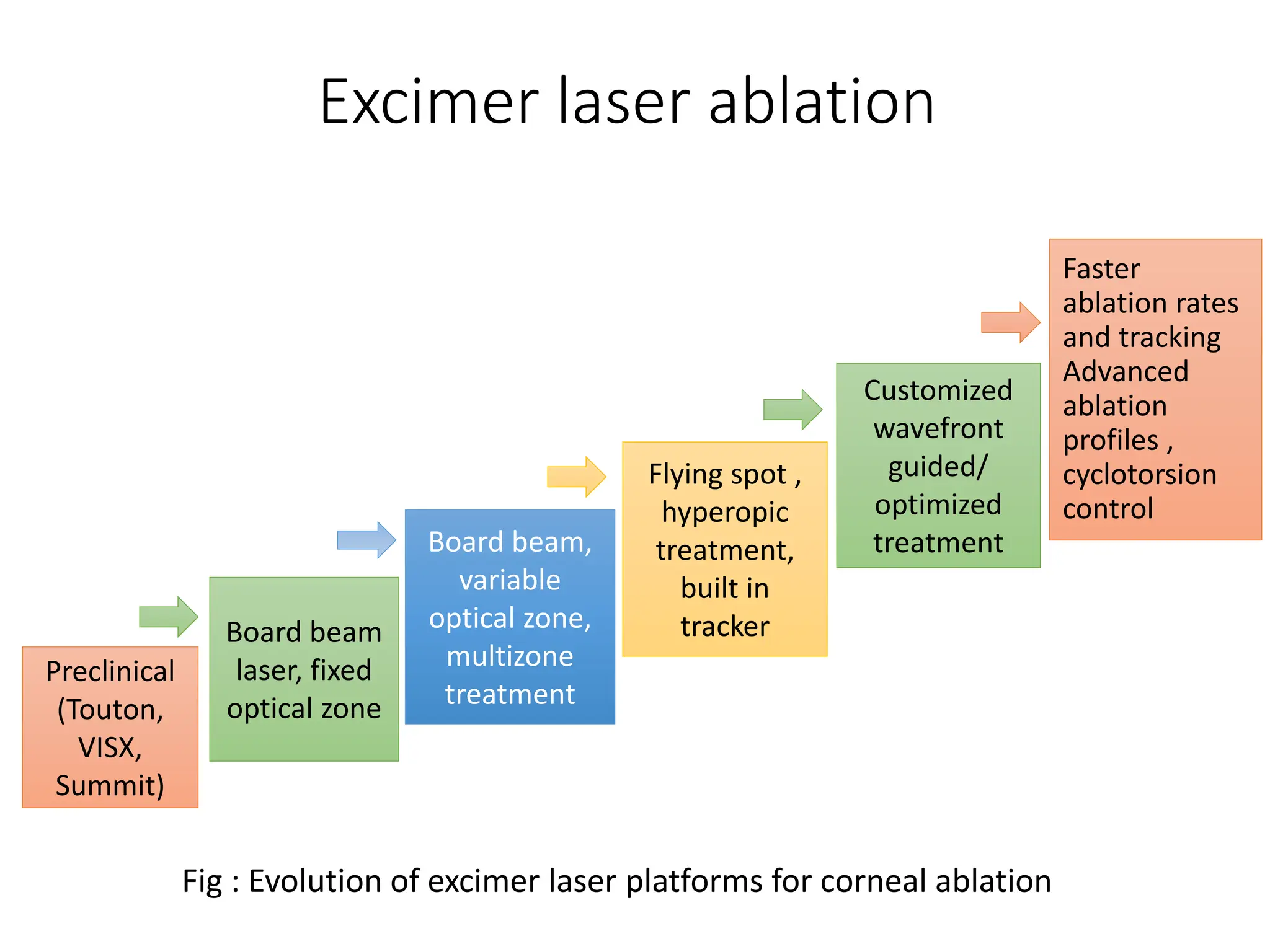
The document discusses refractive surgeries for myopia, detailing principles, types, procedures, and criteria for eye selection. It outlines the history and classification of various surgical techniques, such as LASIK, PRK, and SMILE, as well as the biomechanical aspects of the cornea and the technological advancements in surgical instruments. Additionally, it examines specific procedures along with their indications, contraindications, and potential complications.
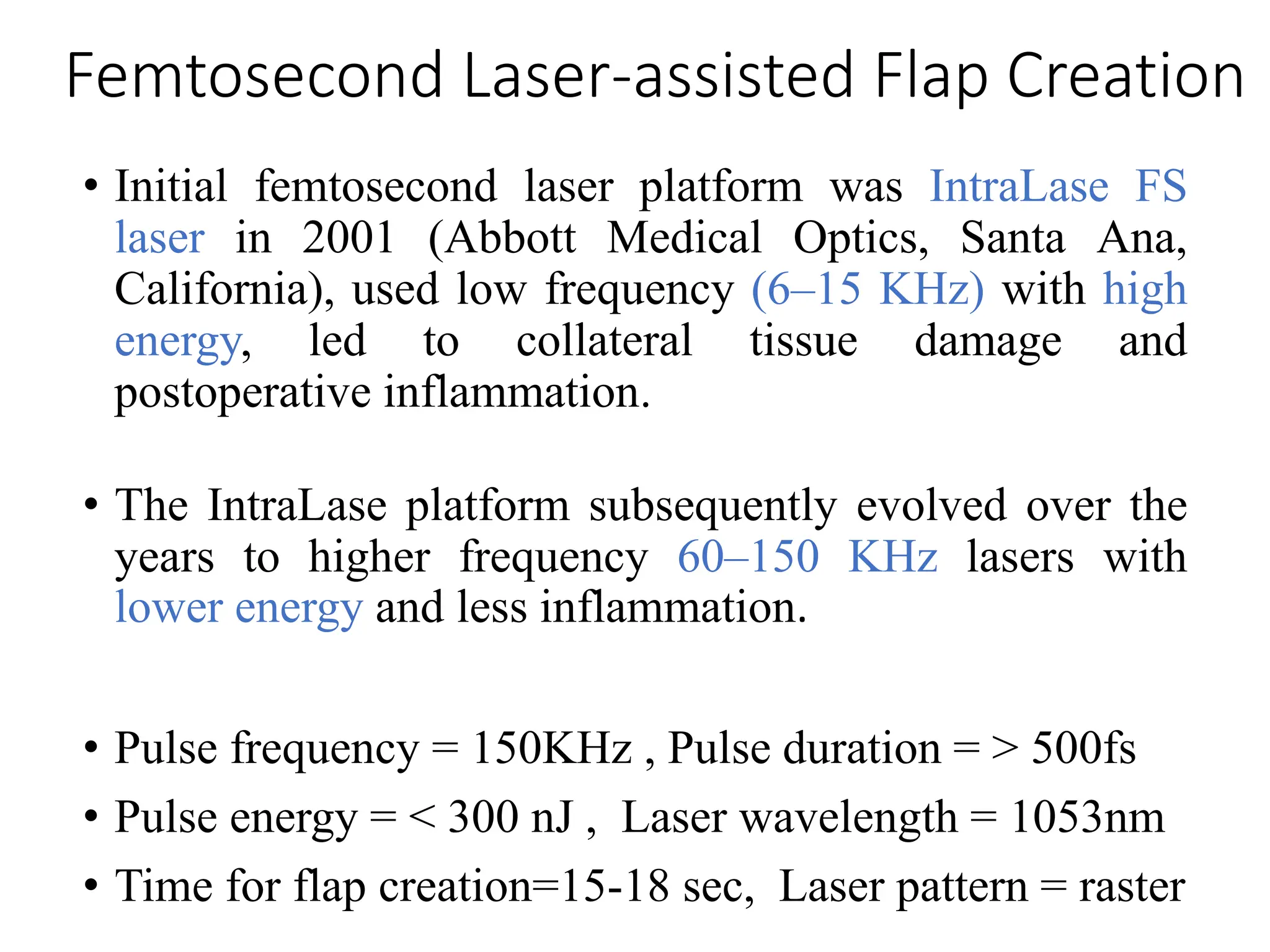
![Excimer laser ablation
Depth of ablation (µm) = [diameter of optical
zone(mm)] 2 × 1/3 power(D)
• An estimate of the ablation
depth during LASIK surgery
is provided by the
Munnerlyn’s equation
• Discovered by Charles
Munnerlyn](https://image.slidesharecdn.com/refractivesurgery-a-240616124628-881650bc/75/Refractive-Surgery-Principle-Selection-of-eyes-Instruments-Procedures-for-myopia-31-2048.jpg)