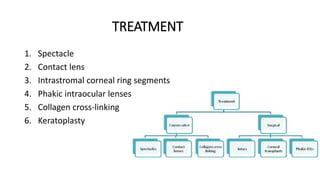
This document provides an overview of keratoconus, including its epidemiology, etiology, pathology, clinical presentation, diagnostic evaluation, and treatment options. Keratoconus is a non-inflammatory thinning of the cornea that can be diagnosed using topography to detect corneal steepening and irregularity. While its cause is unknown, risk factors include eye rubbing and family history. Treatment may involve spectacles, contact lenses, intrastromal corneal ring segments, phakic intraocular lenses, or collagen cross-linking to prevent progression, with keratoplasty as a last option. Newer treatments like intracorneal ring segments and collagen cross-linking have expanded options to better treat and even arrest progression of keratocon