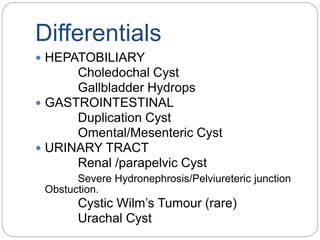
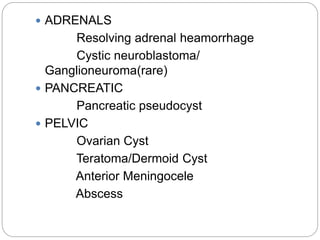
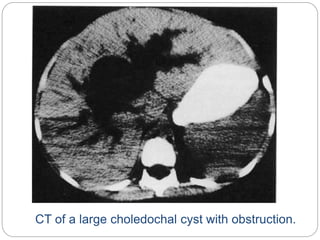
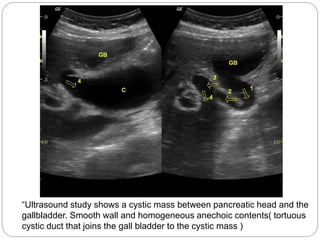
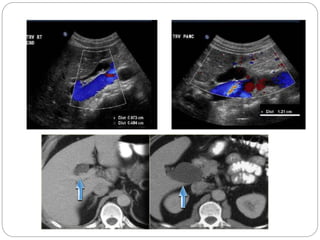
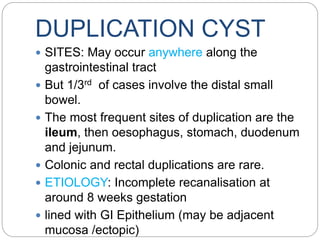
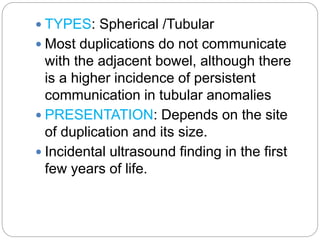
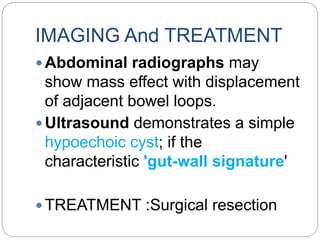
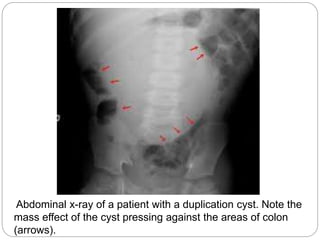
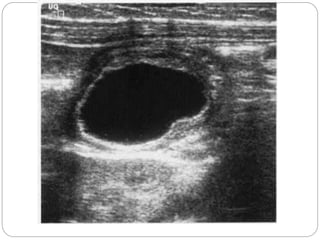
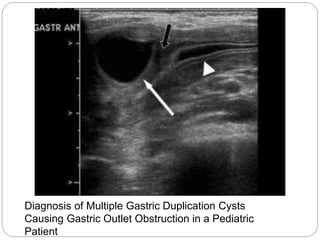
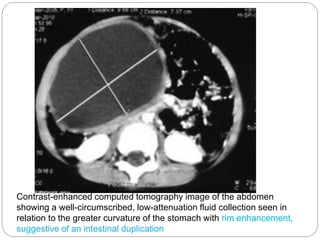
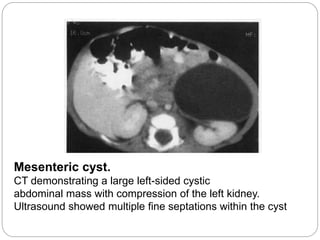
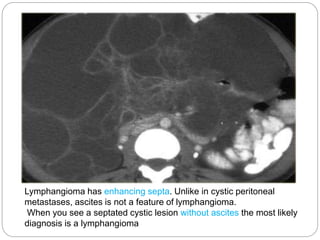
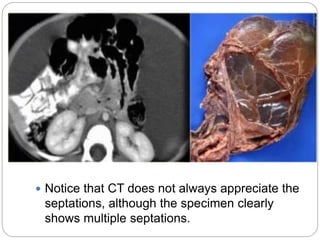
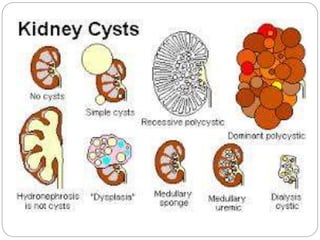
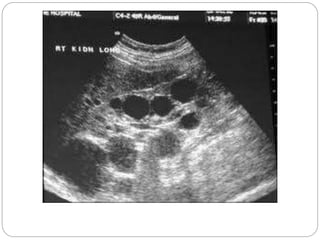
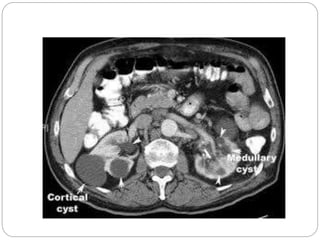
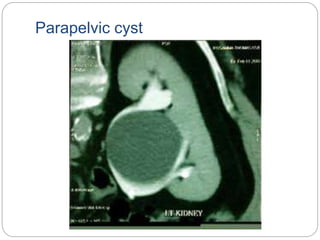
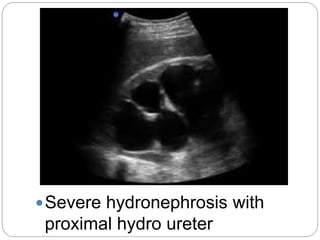
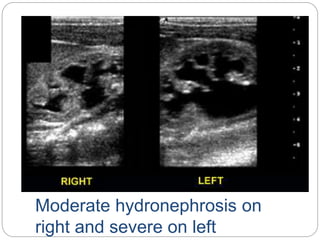
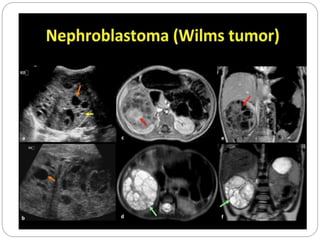
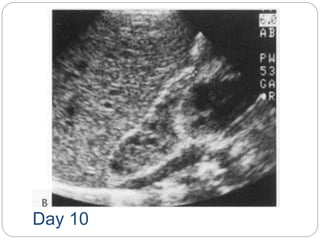
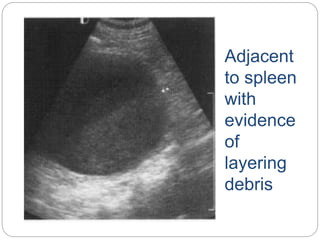
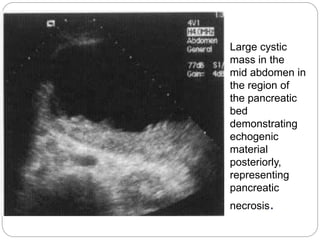
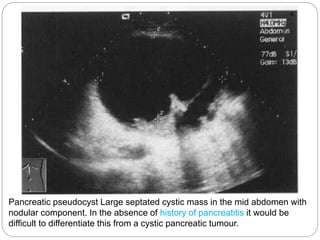
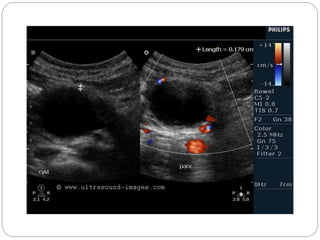
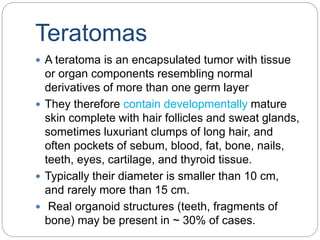
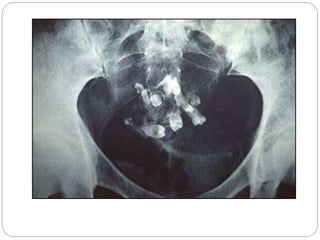
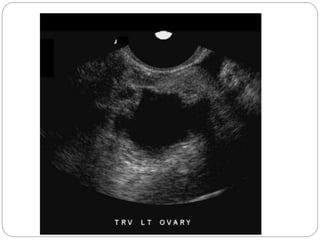
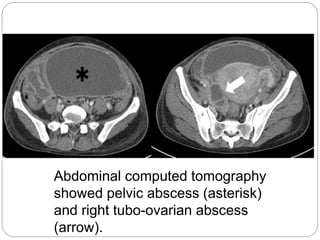
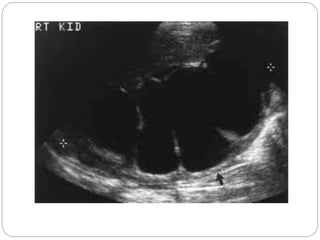
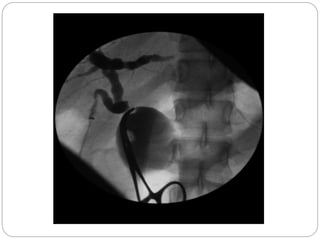
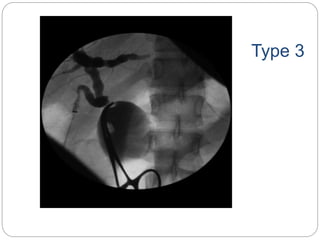
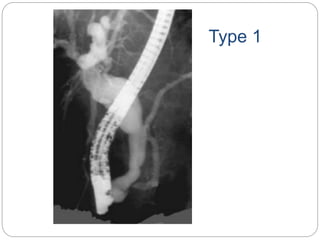
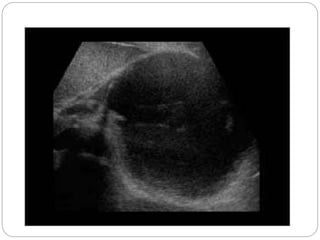
This document discusses different types of intra-abdominal cysts that can occur in children. It describes cysts arising in the hepatobiliary system like choledochal cysts and gallbladder hydrops. Gastrointestinal cysts such as duplication cysts and omental/mesenteric cysts are also reviewed. Other cysts discussed include renal, adrenal, pancreatic, ovarian and pelvic cysts. For each type, the document provides details on etiology, imaging appearance and differential diagnosis to help in evaluating cystic masses found in pediatric abdominal imaging studies.