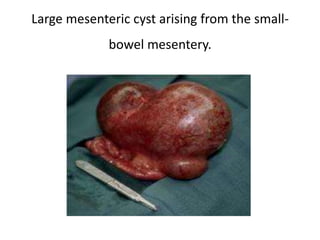
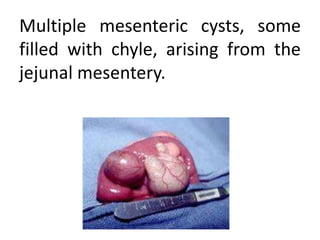
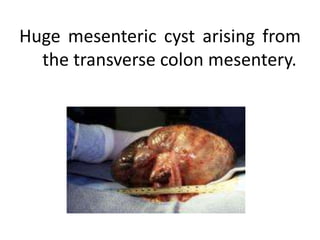
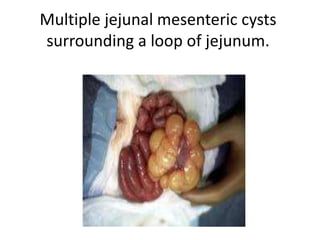
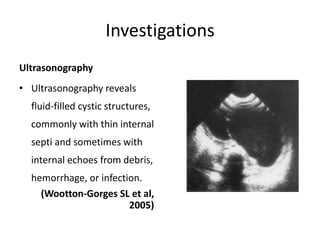
Mesenteric cysts are rare abdominal masses formed by fluid collections in the small bowel mesentery and can vary in size and type, ranging from simple to complex structures. Diagnosis is primarily through ultrasonography, and treatment typically involves surgical options such as enucleation, resection, or marsupialization, depending on the size and location of the cyst. Postoperative care is critical, with good long-term outcomes and a low recurrence rate; early diagnosis can help prevent complications related to intestinal obstruction.