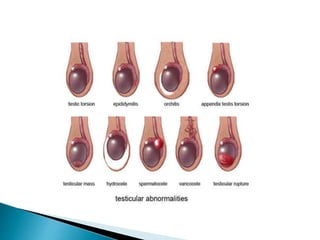
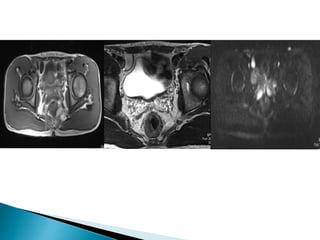
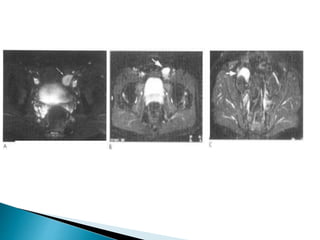
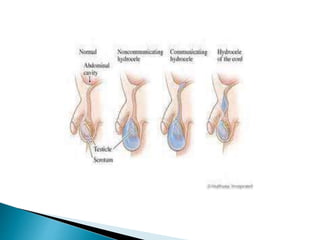
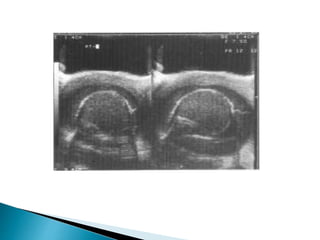
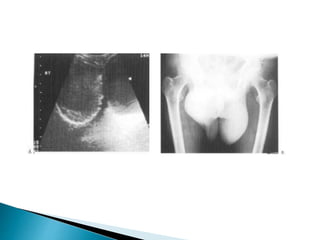
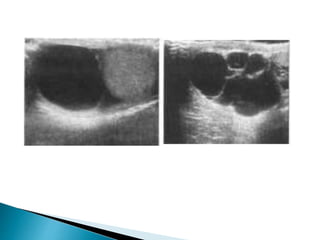
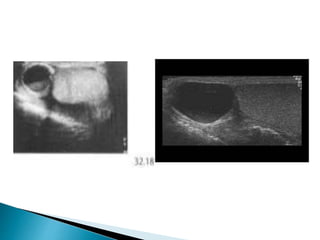
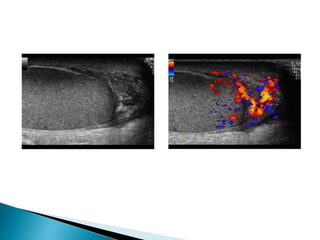
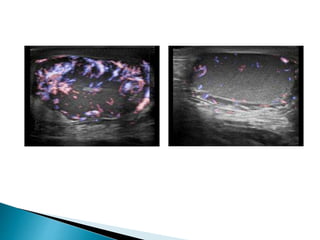
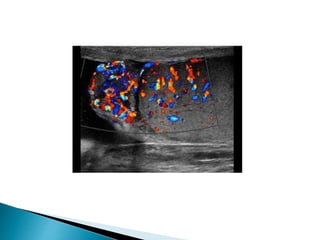
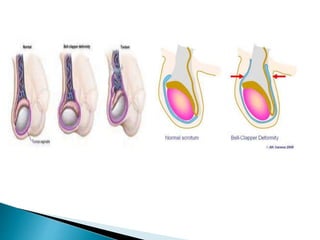
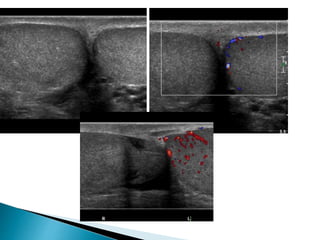
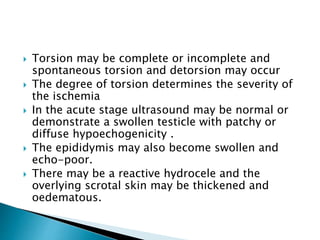
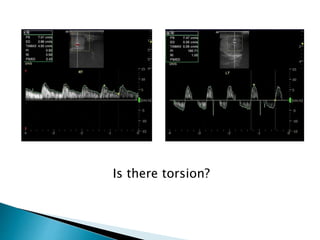
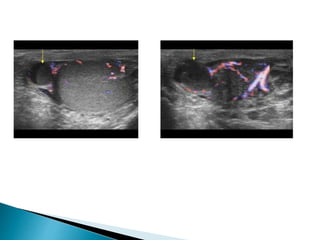
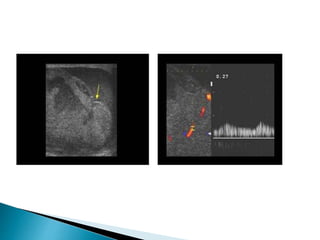
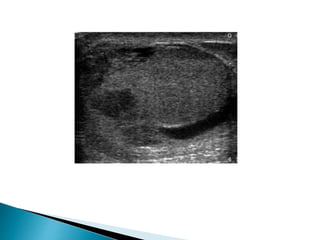
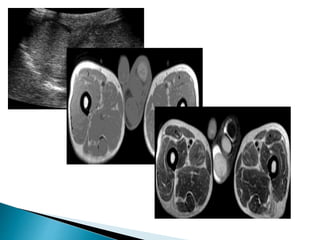
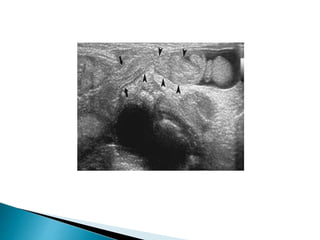
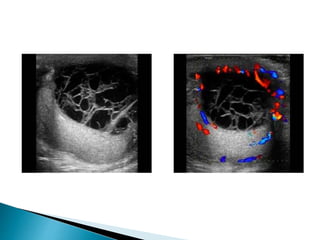
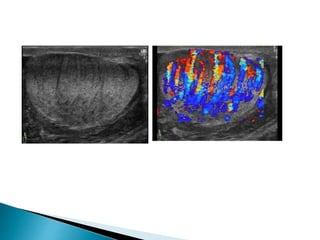
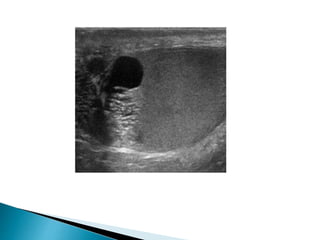
This document discusses various disorders of the scrotum and testes that can be evaluated with ultrasound imaging. It covers congenital anomalies like undescended testes, acquired conditions like hydrocele and epididymitis, and traumatic injuries. Ultrasound is described as the preferred method for diagnosing these conditions by identifying features like cysts, swelling, blood flow changes, and ruptures. Timely ultrasound exams are important for urgent issues like testicular torsion.