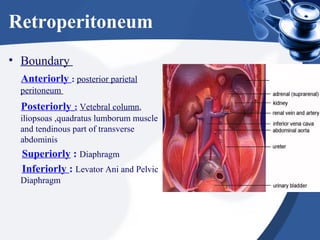
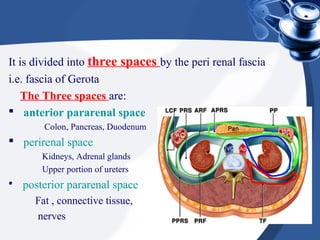
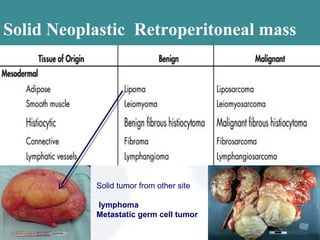
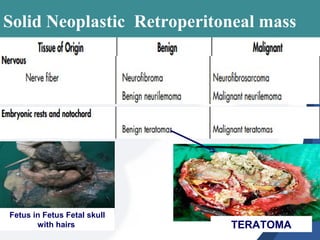
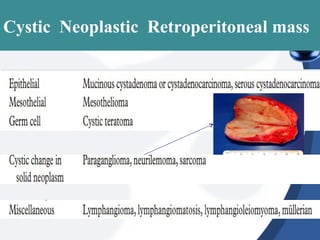
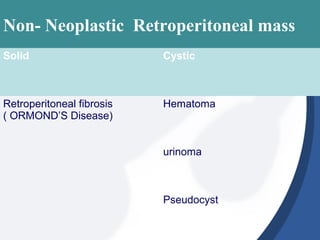
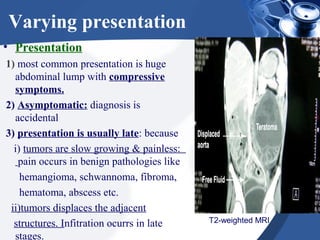
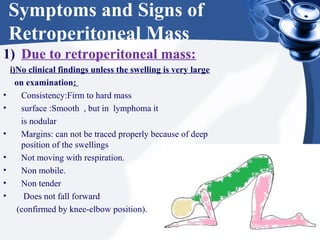
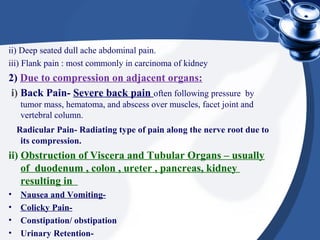
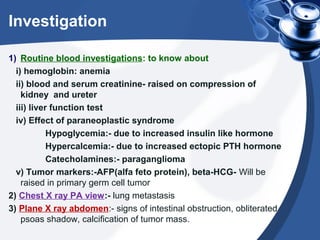
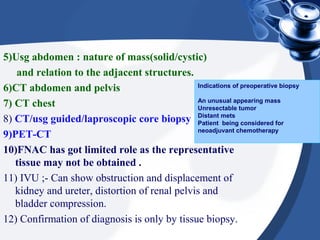
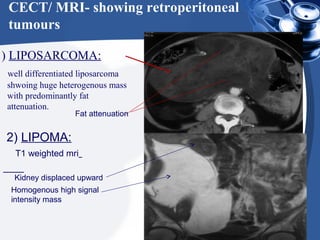
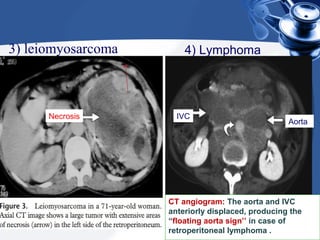
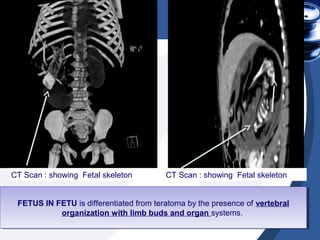
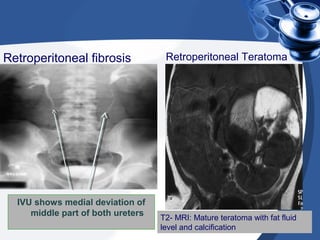
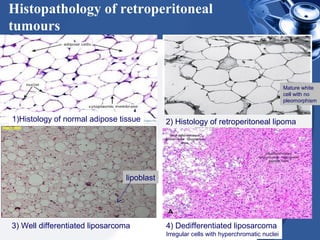
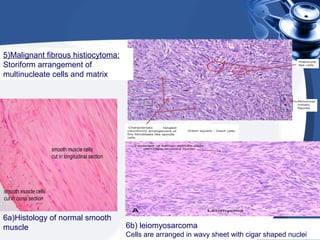
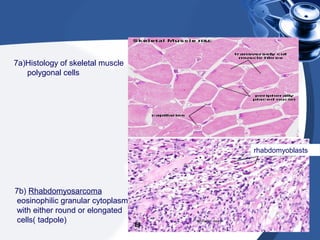
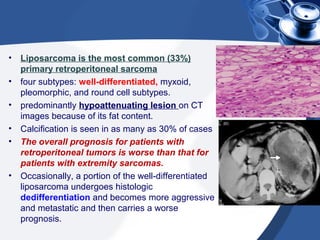
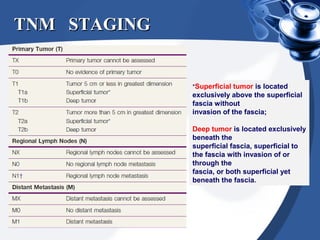
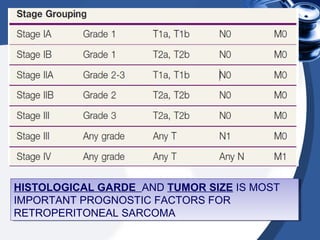
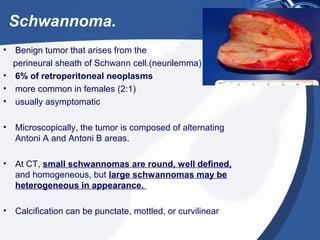
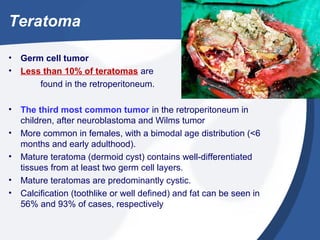
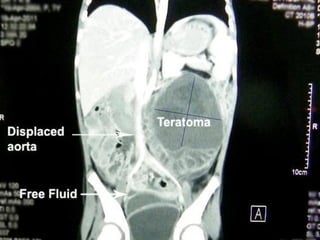
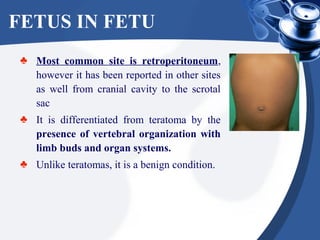
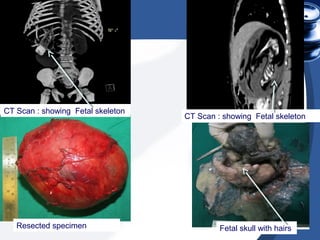
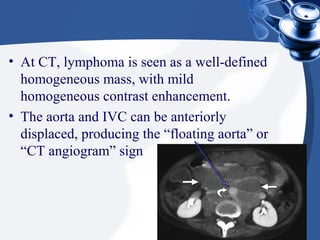
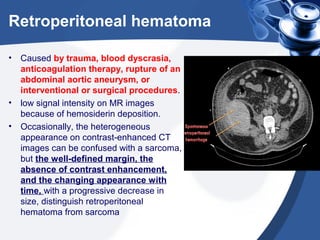
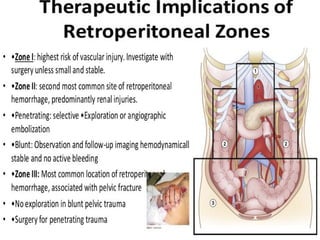
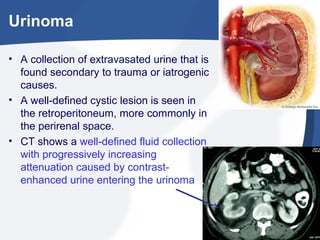
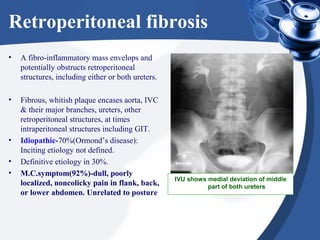
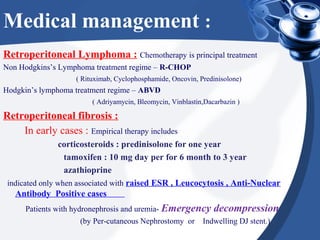
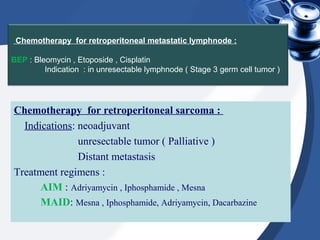
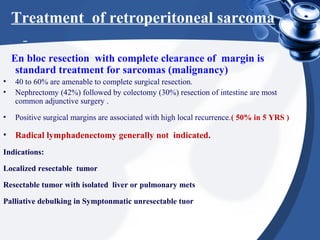
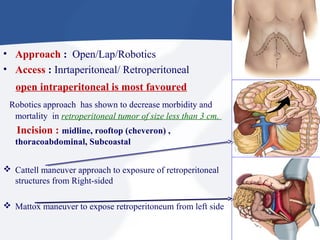
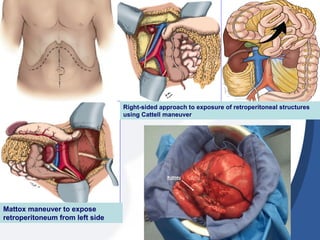
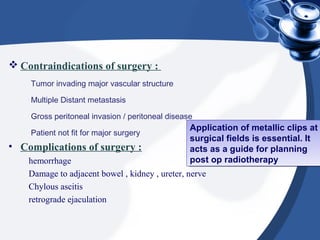
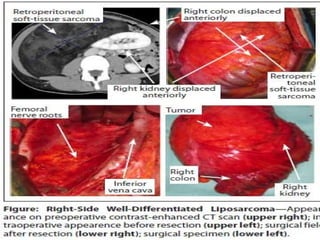
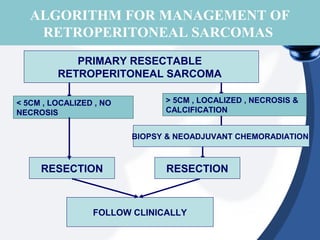
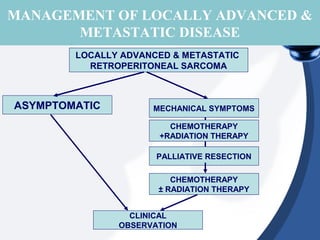
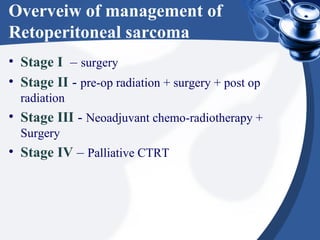
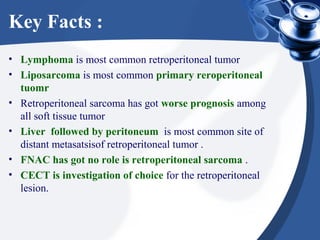
The document provides a comprehensive overview of retroperitoneal masses, including their etiology, clinical presentations, and management strategies. It discusses the anatomical spaces, types of masses such as neoplastic and non-neoplastic formations, relevant investigations, and treatment options including surgical and medical interventions. Additionally, it emphasizes the importance of biopsy for diagnosis and outlines management protocols based on tumor staging.