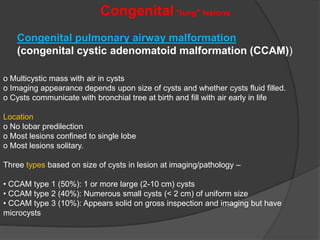
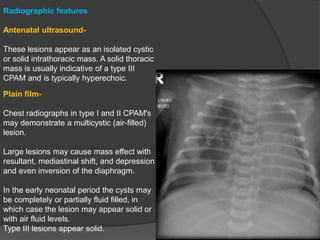
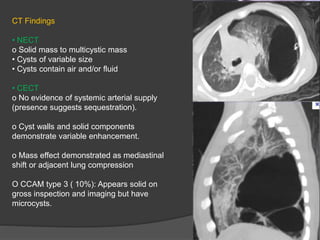
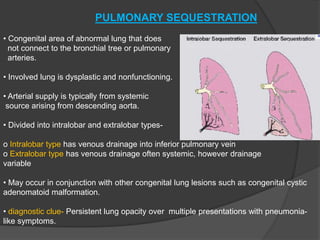
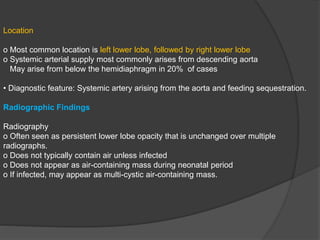
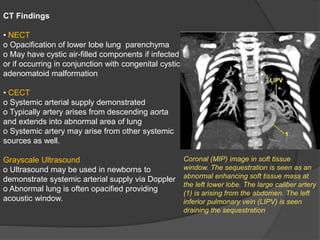
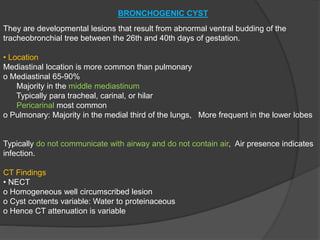
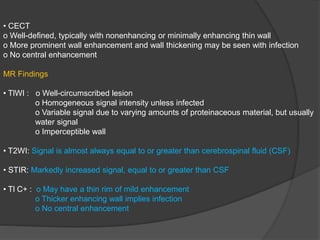
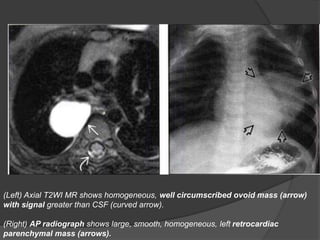
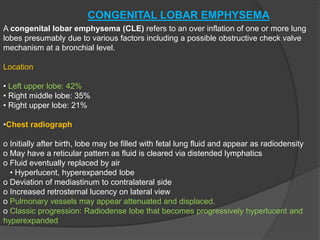
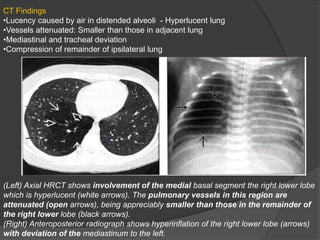
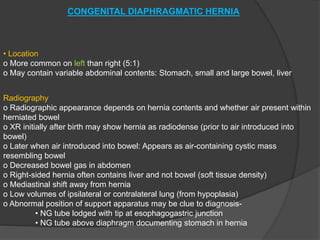
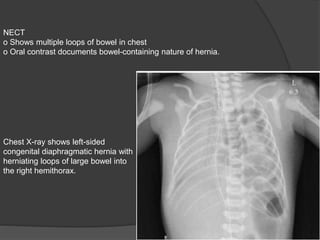
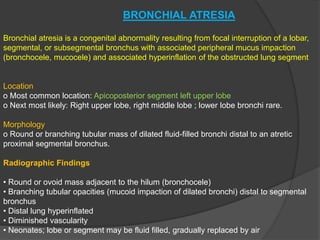
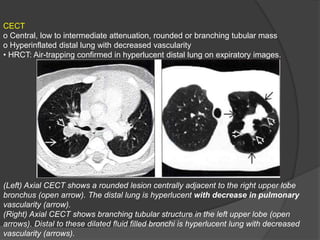
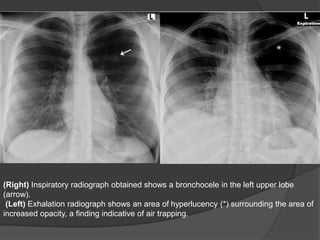
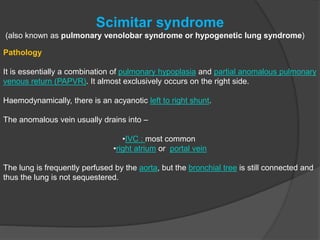
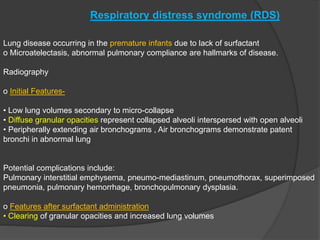
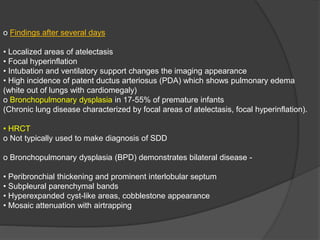
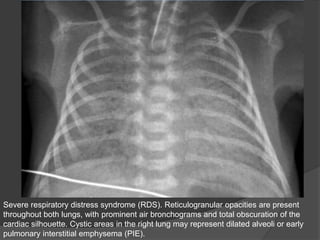
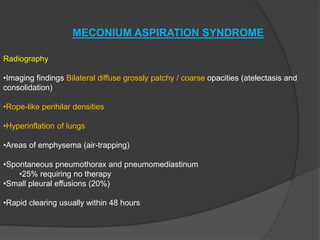
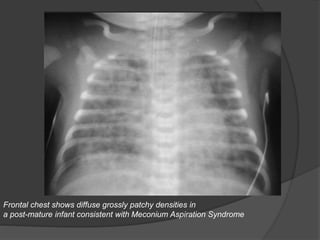
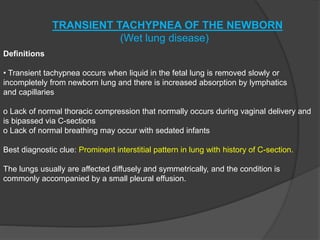
This document discusses several congenital lung lesions and neonatal chest issues seen in infants. It provides descriptions of cystic adenomatoid malformation, pulmonary sequestration, bronchogenic cyst, congenital lobar emphysema, congenital diaphragmatic hernia, and bronchial atresia. For each condition, it summarizes the location, radiographic features on imaging such as x-ray and CT, and pathological findings. It also briefly discusses other neonatal issues like surfactant deficient disease and meconium aspiration syndrome.