The document discusses regeneration, repair, and the roles of stem cells and the extracellular matrix in the processes. It makes the following key points:
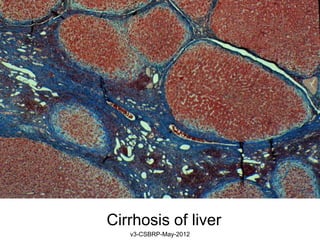
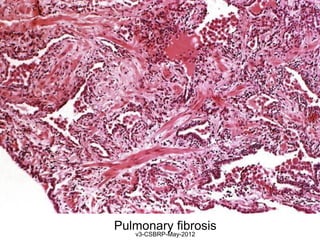
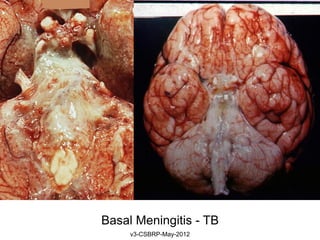
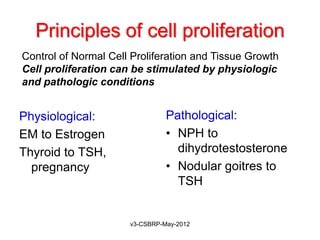
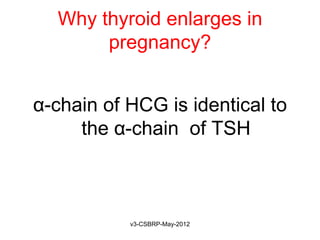
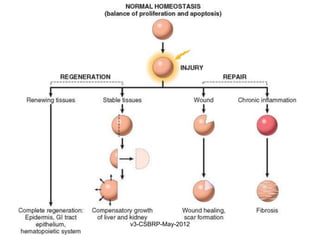
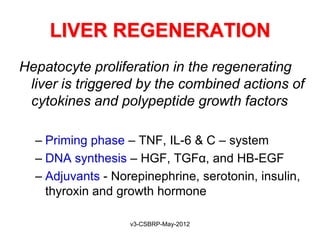
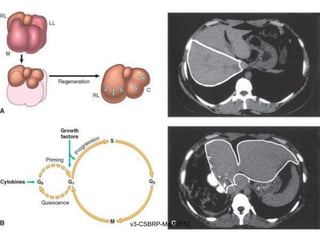
1. Regeneration refers to the proliferation of cells and tissues to replace lost structures, while repair is a healing process involving regeneration and scar formation.
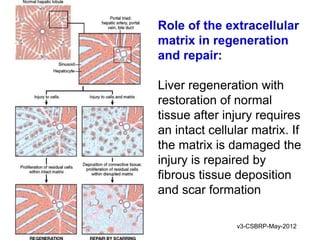
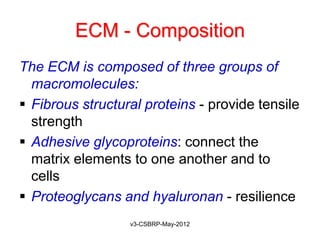
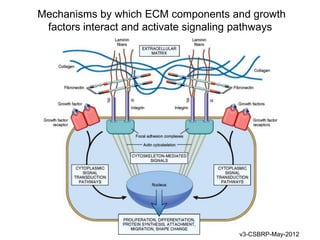
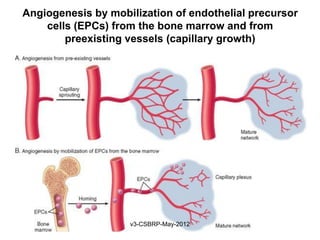
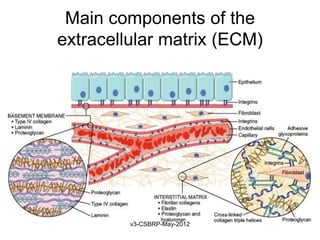
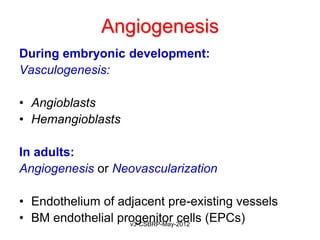
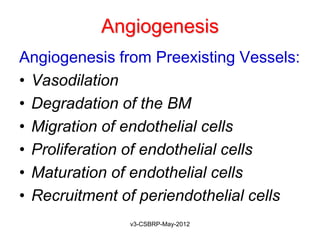
2. The extracellular matrix is essential for wound healing by providing structure for cell migration and facilitating angiogenesis and growth factor production.
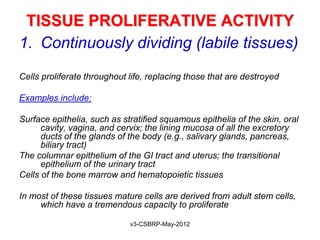
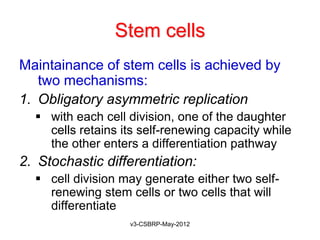
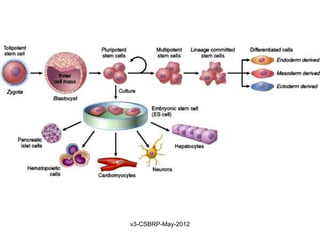
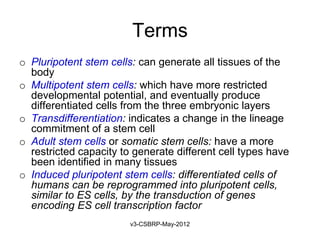
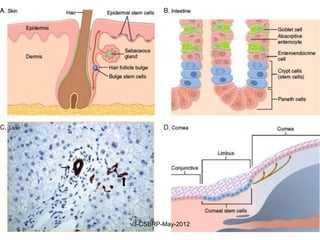
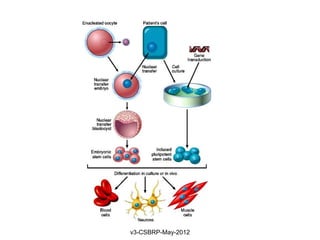
3. Stem cells maintain tissues through self-renewal and differentiation. Adult stem cells support regeneration in tissues like liver, skin, and blood.