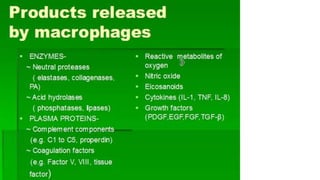
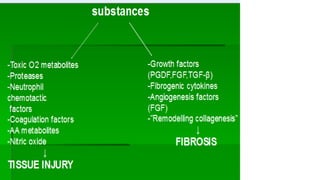
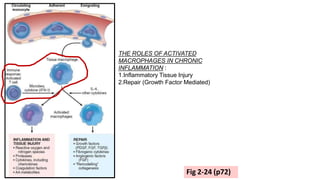
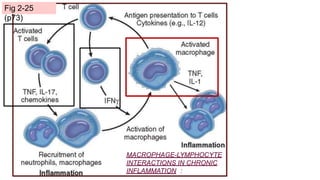
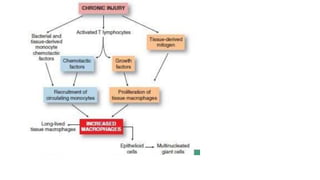
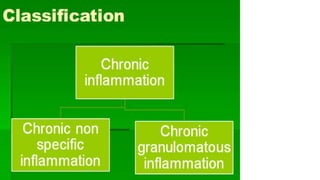
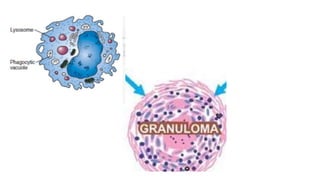
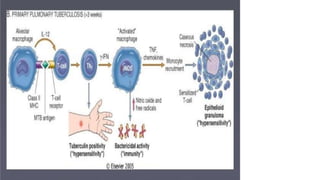
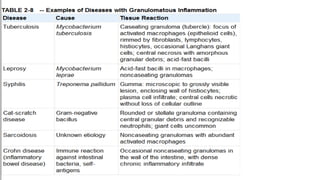
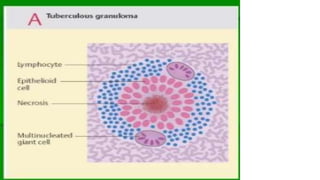
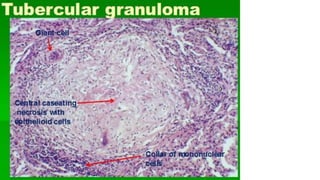
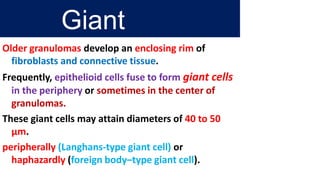
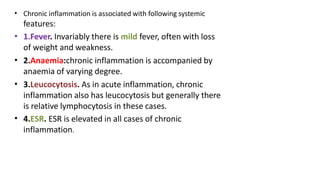
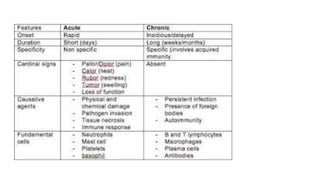
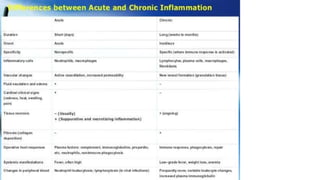
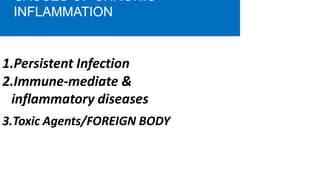
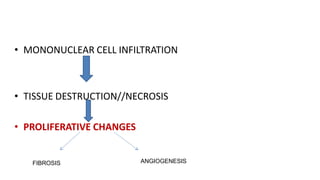
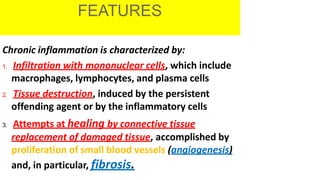
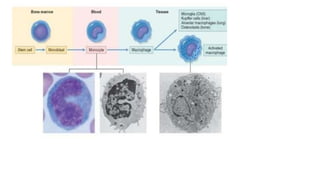
Chronic inflammation is characterized by prolonged inflammation lasting weeks or months, where inflammation, tissue injury, and repair occur simultaneously. It is caused by persistent infections, immune-mediated diseases, or toxic agents. Chronic inflammation involves infiltration of mononuclear cells like macrophages and lymphocytes, ongoing tissue destruction, and attempts at repair through fibrosis and angiogenesis. Macrophages play a key role by secreting cytokines and growth factors that mediate both inflammatory tissue injury and repair.



![• CYTOKINES-IL1, IL-2
• INTERFERONS –Y
• GROWTH FACTORS- TGF, PDGF, FGF,EGF
• [TGF, PDGF------- to stimulate fibroblast]
• COMPLEMENT FACTORS[C]
• ENZYMES—Proteases, endonucleases,
elastases](https://image.slidesharecdn.com/class3ci-230619143211-e63c2689/85/CLASS-3-CI-pptx-15-320.jpg)
![• IS NORMAL LYMPHOCYTE SECRETES
LYMPHOKINES??
• CD4 Lymphocytes[[Th cells]](https://image.slidesharecdn.com/class3ci-230619143211-e63c2689/85/CLASS-3-CI-pptx-18-320.jpg)