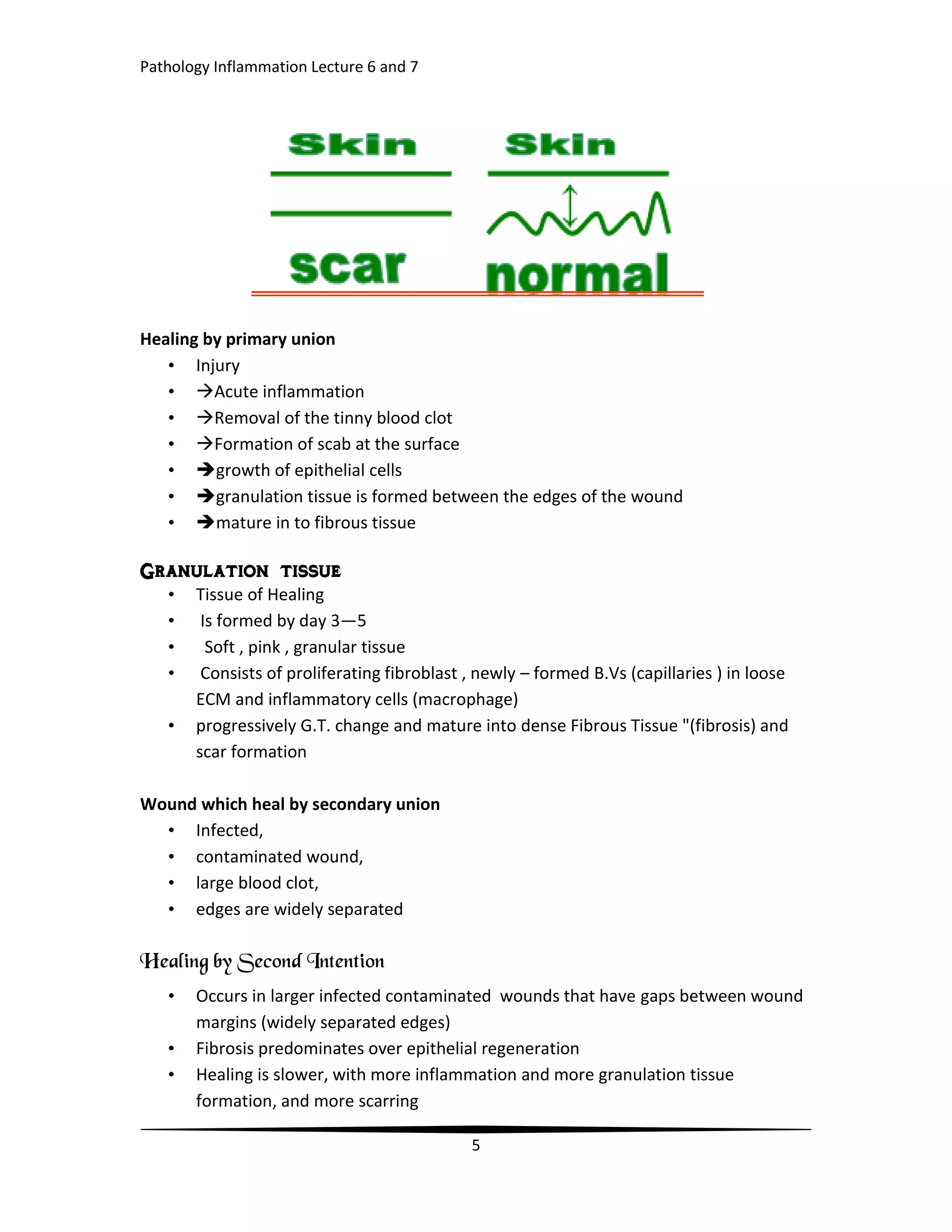
1. Tissue repair occurs through regeneration or healing. Regeneration replaces dead cells with the same cell type, while healing replaces tissue with fibrous scar tissue.
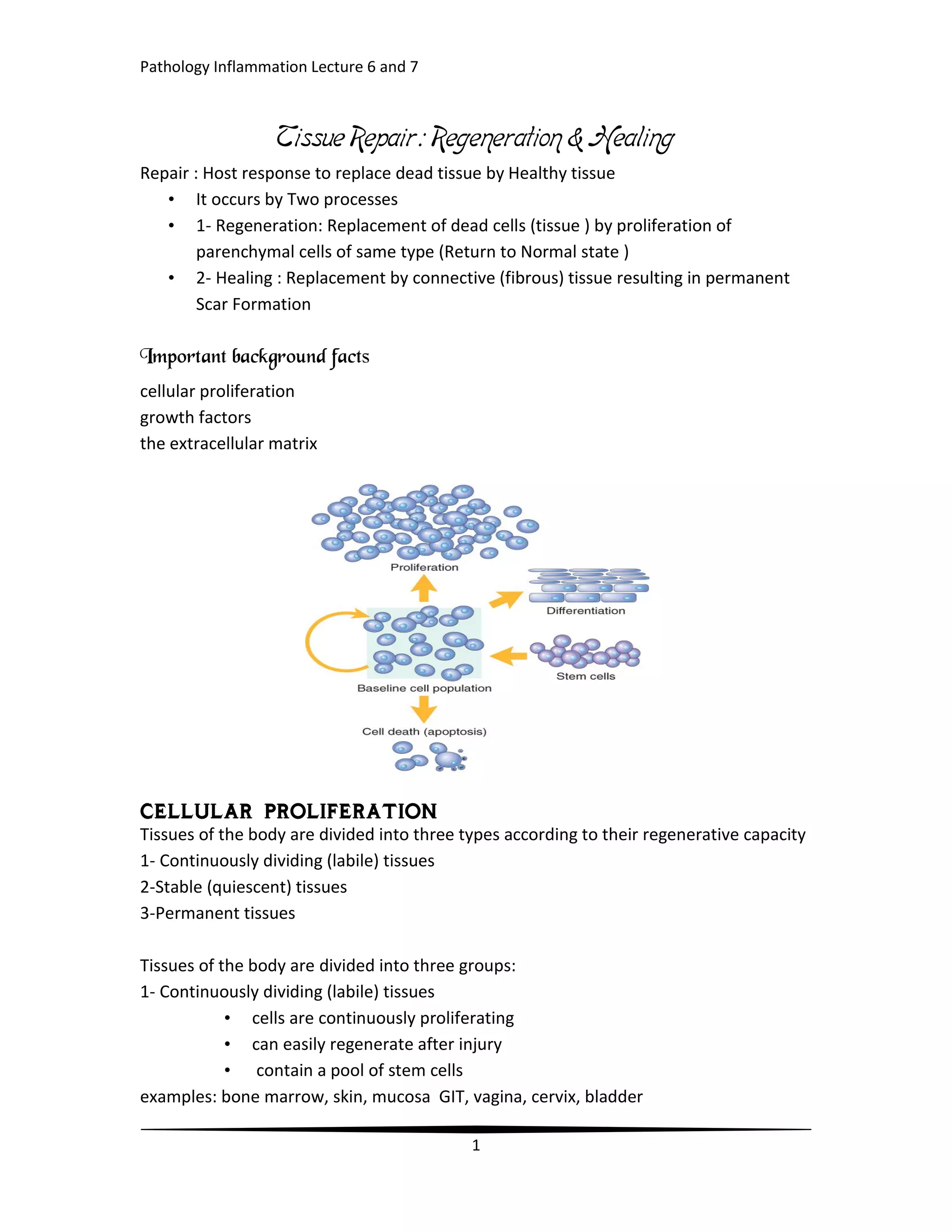
2. The regenerative capacity of tissues depends on their ability to proliferate. Labile tissues continuously divide, stable tissues stop dividing after birth but can proliferate in response to injury, and permanent tissues stop dividing early in life.
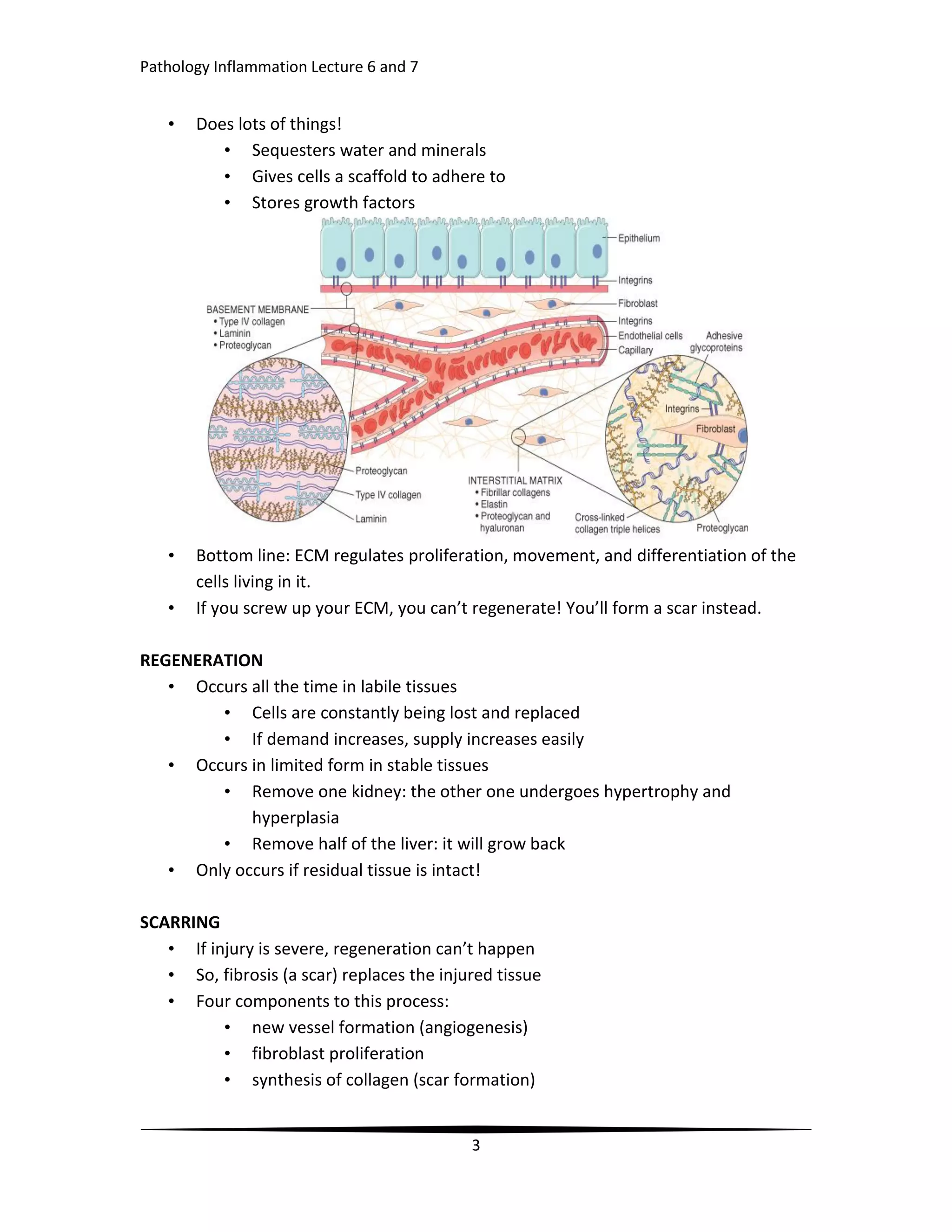
3. Growth factors, the extracellular matrix, and cellular proliferation play important roles in tissue repair by stimulating cell growth, promoting cell survival, and providing a scaffold for cells.