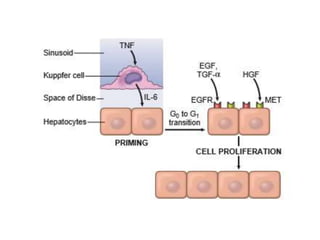
This document summarizes several factors that influence tissue repair and regeneration. It discusses how infection, diabetes, nutritional status, glucocorticoids, mechanical factors, poor perfusion, foreign bodies, the type and extent of tissue injury, and the location of the injury can impact healing. It also provides details on liver regeneration through the proliferation of remaining hepatocytes or repopulation from progenitor cells after partial hepatectomy. The regeneration process involves three phases: priming, growth factor stimulation, and termination.