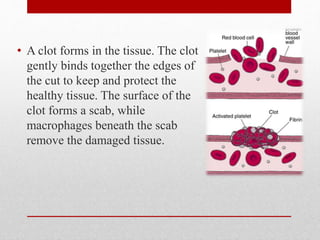
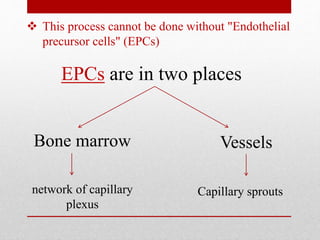
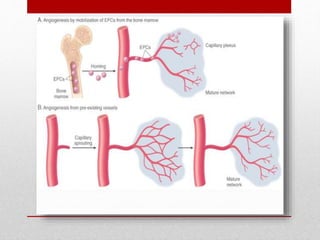
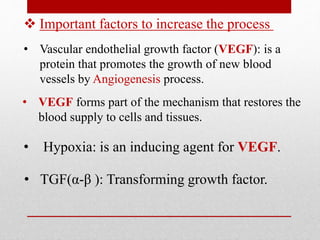
Tissue repair occurs through regeneration, replacing damaged cells with the same cell type, or fibrosis, replacing tissue with scar tissue. During fibrosis, blood vessels bleed and mast cells release histamine to promote vasodilation. A clot forms while macrophages remove damaged tissue. Fibroblasts migrate in and produce collagen, forming scar tissue through angiogenesis, fibroblast migration and proliferation, extracellular matrix deposition, and remodeling. Vascular endothelial growth factor is important for angiogenesis and permeability while transforming growth factor promotes fibroblast migration.