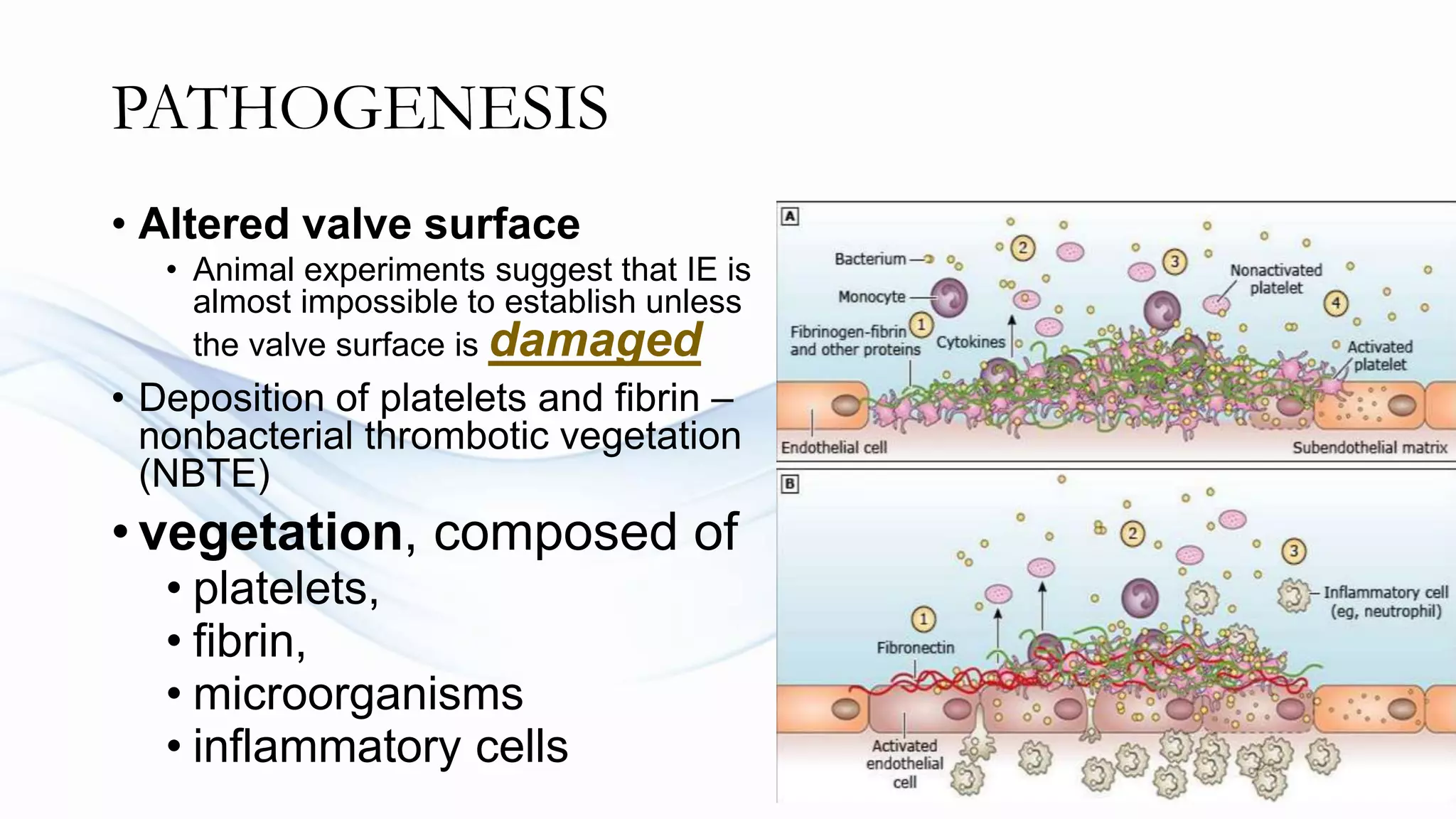
Infective endocarditis is a microbial infection of the heart valves or endocardium. It can be acute or subacute depending on the virulence of the organism and host factors. Common symptoms include fever, heart murmur, and embolic phenomena. Diagnosis involves blood cultures, echocardiogram, and applying the Duke criteria. Treatment is with prolonged antibiotic therapy tailored to the identified organism. Surgery may be needed for complications or uncontrolled infection. Infective endocarditis has a high mortality rate around 25% depending on the organism and underlying heart condition.


















![Sub-Acute IE
Untreated or partially treated for weeks and
months
Bacteria -> Releases antigen for prolong time
= chronic antigenemia
Antigen-antibody complexes are formed
While Circulating gets deposited in the
microcirculation
Complements are activated and damages local
tissues [type 3 hypersensitivity]
Vasculitic lesion are formed](https://image.slidesharecdn.com/infendocarditis-230214084353-88767831/75/infectious-endocarditis-pptx-21-2048.jpg)





















