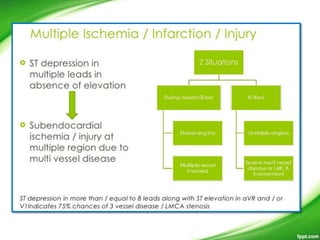
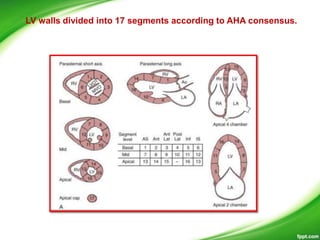
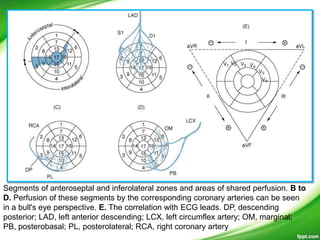
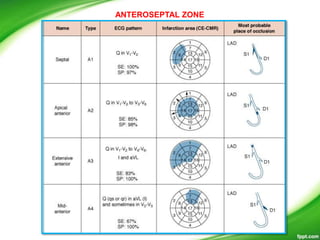
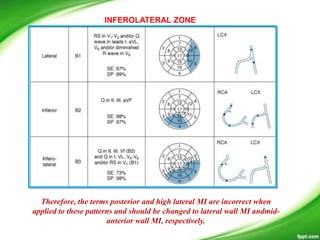
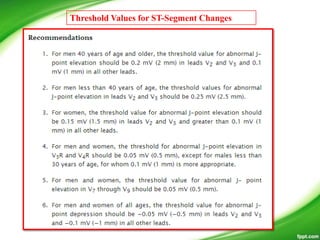
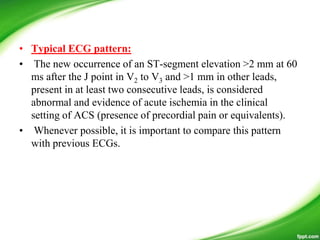
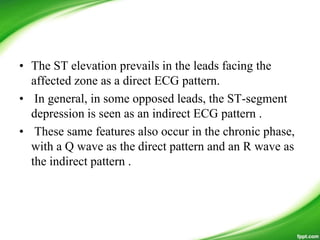
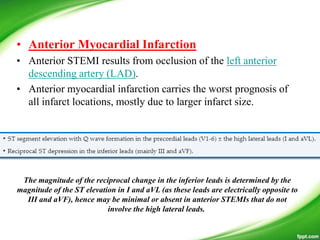
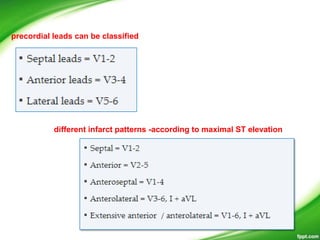
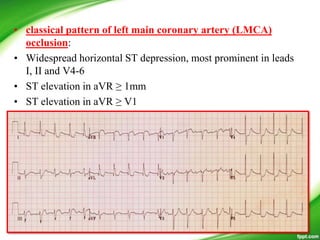
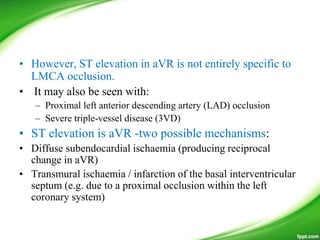
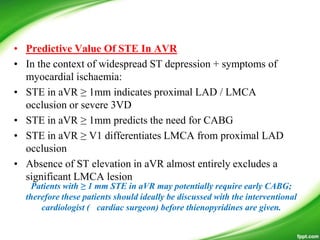
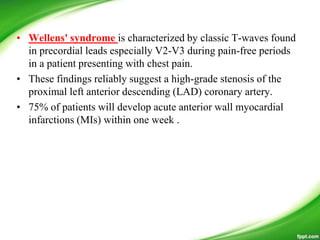
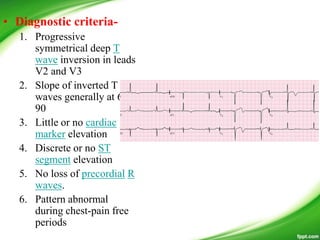
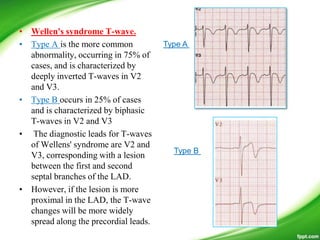
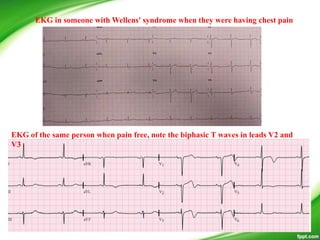
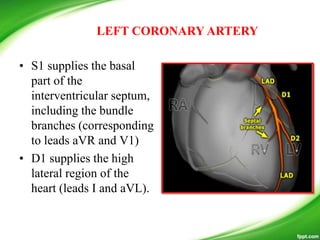
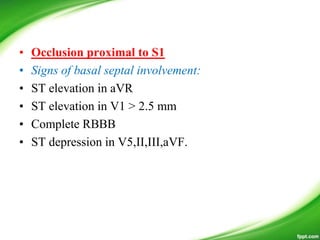
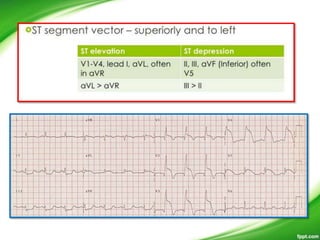
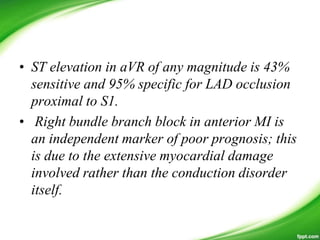
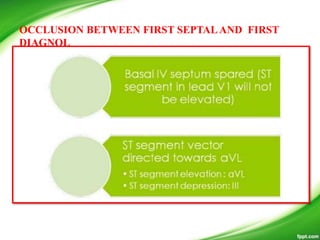
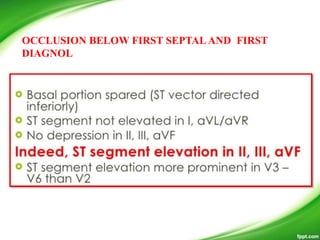
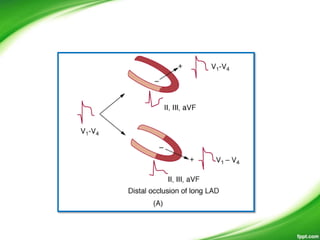
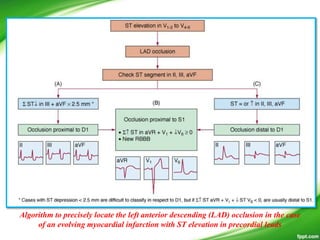
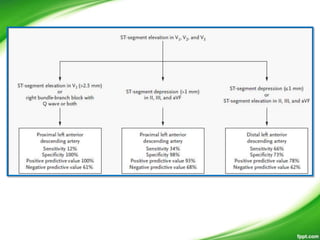
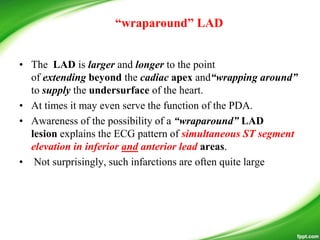
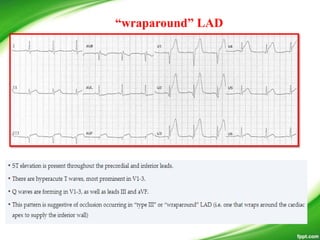
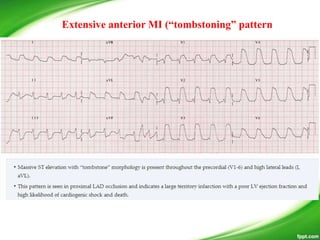
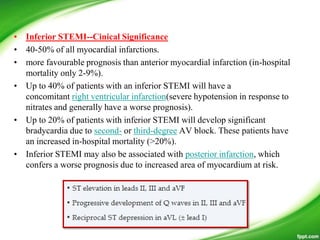
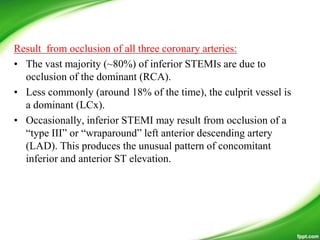
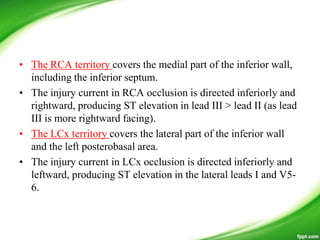
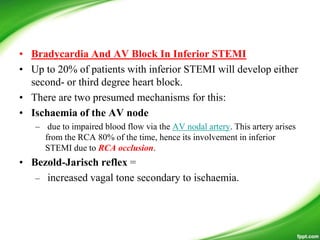
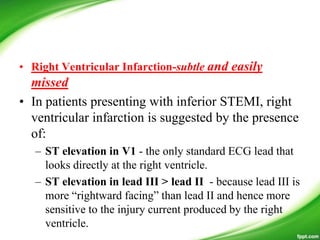
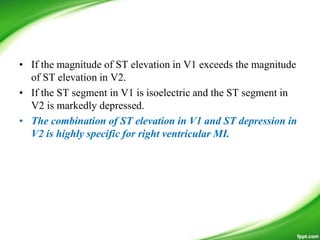
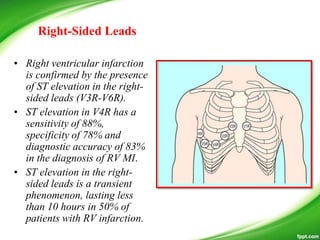
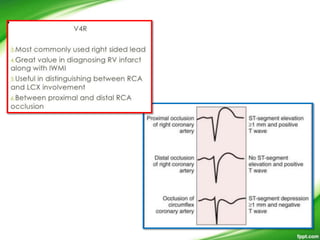
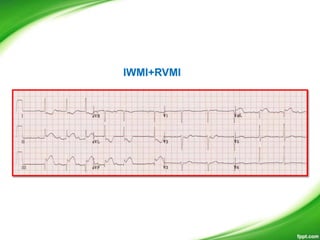
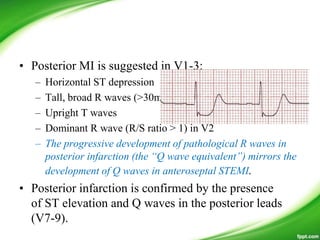
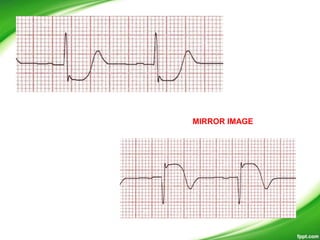
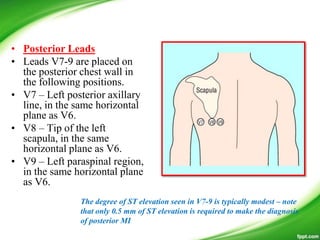
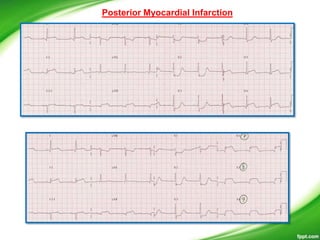
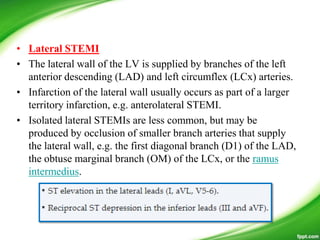
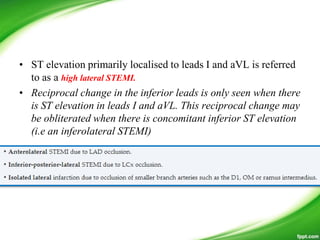
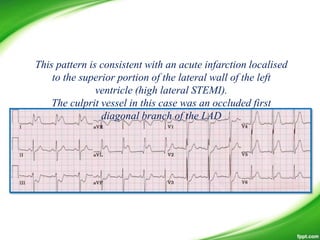
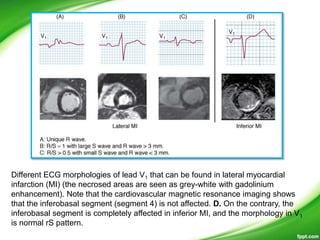
This document discusses ECG patterns in ST-elevation acute coronary syndrome (ACS). It provides threshold values for defining ST elevation and discusses patterns corresponding to different infarct locations. Anterior STEMI results from LAD occlusion and involves the interventricular septum. Inferior STEMI is usually due to RCA occlusion but can also be from dominant LCx occlusion. Wellens' syndrome indicates high-grade LAD stenosis. Posterior MI accompanies inferior or lateral MI and implies a larger infarct size. The document also provides algorithms to localize the infarct artery based on ECG patterns.
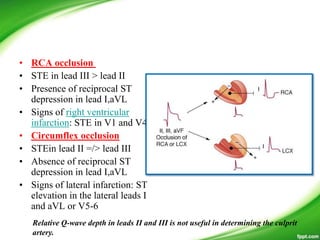
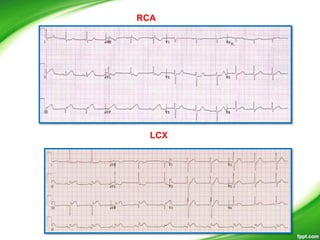
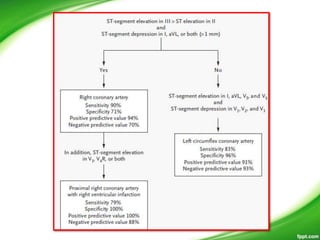
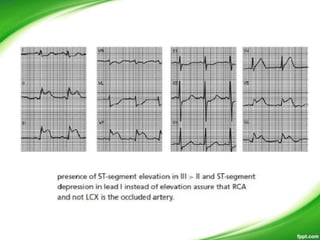
![Algorithm to predict the culprit artery (right
coronary artery [RCA] vs left circumflex artery
[LCX]) in case of evolving myocardial
infarction with ST elevation in inferior leads](https://image.slidesharecdn.com/infarctlocalisation-140413073837-phpapp02/85/Infarct-localisation-50-320.jpg)
![Algorithm to predict the culprit artery (right
coronary artery [RCA] vs left circumflex artery
[LCX]) in case of evolving myocardial
infarction with ST elevation in inferior leads](https://image.slidesharecdn.com/infarctlocalisation-140413073837-phpapp02/85/Infarct-localisation-51-320.jpg)