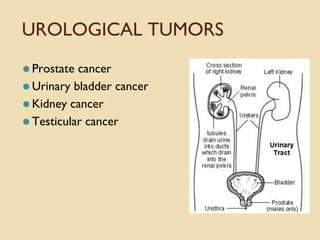
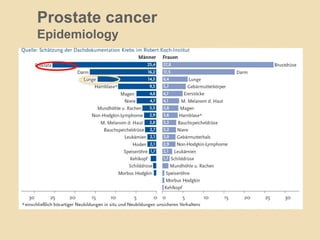
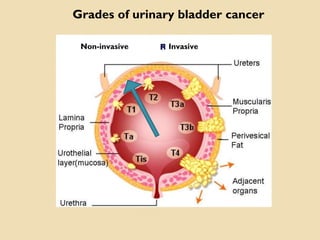
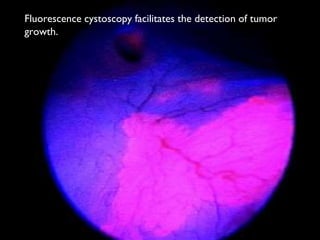
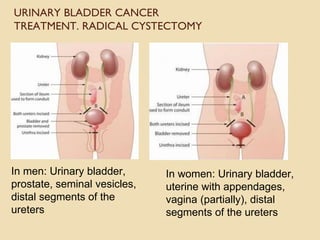
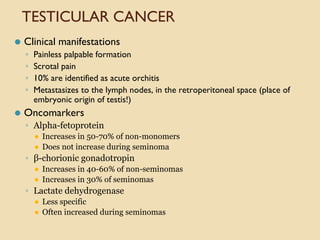
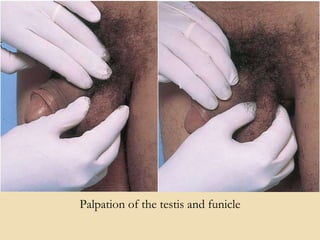
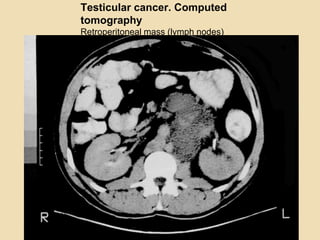
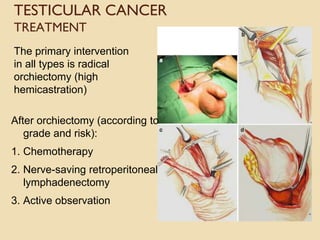
This document discusses various urological tumors including prostate cancer, urinary bladder cancer, kidney cancer, and testicular cancer. It provides information on the epidemiology, risk factors, clinical presentation, diagnosis, and treatment options for each type of cancer. The key points are that prostate cancer is the most common cancer in men, urinary bladder cancer is usually transitional cell carcinoma, kidney cancer is often renal cell carcinoma, and testicular cancer occurs most commonly in men ages 30-40. The document outlines the anatomy, pathophysiology, diagnostic tests and imaging, as well as surgical and other therapeutic approaches for each urological tumor type.