This document discusses hospital acquired infections (HAIs), also known as nosocomial infections. Some key points:
- HAIs affect around 2 million people in the US each year, resulting in about 90,000 deaths.
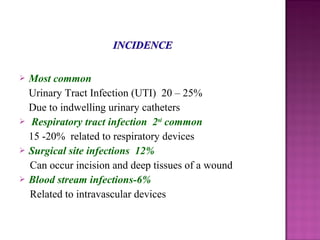
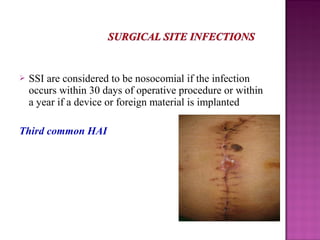
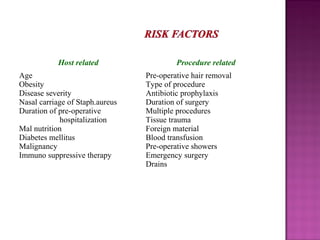
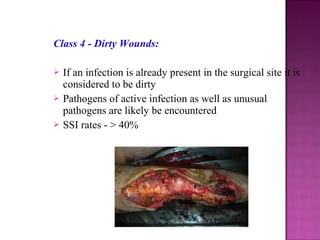
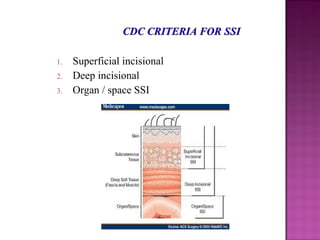
- Common types of HAIs include urinary tract infections, respiratory infections, and surgical site infections.
- HAIs increase mortality, morbidity, and hospital length of stay.
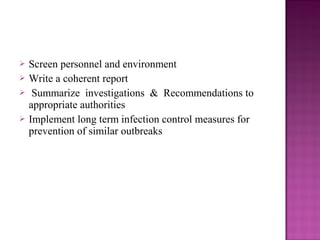
- The chain of infection involves an infectious agent, reservoir, mode of transmission, portal of entry/exit, and susceptible host. Breaking any link can prevent infection.
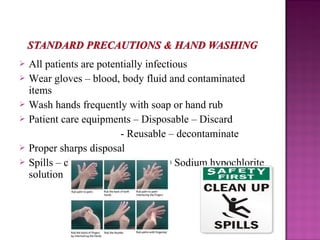
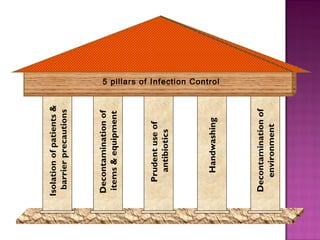
- Strict hand hygiene, isolation precautions, and antibiotic stewardship are essential to control and prevent HAIs.