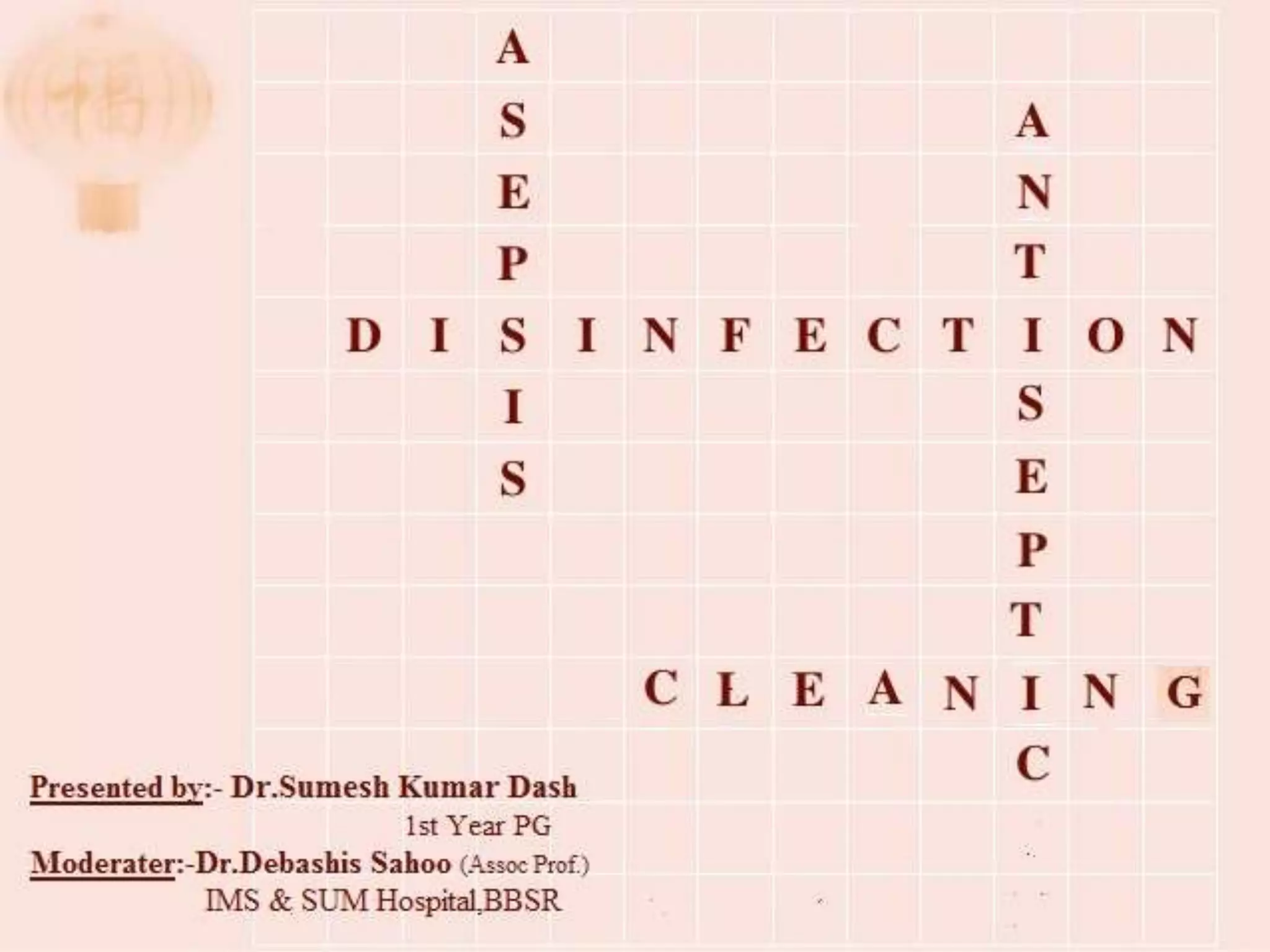
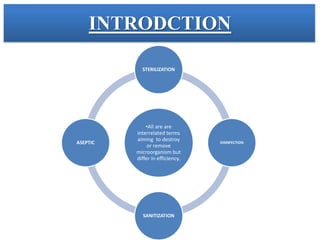
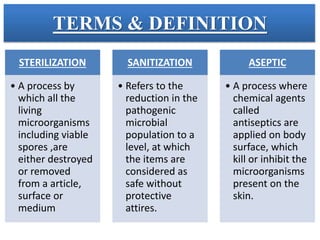
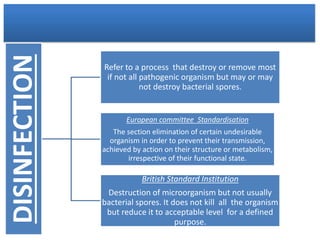
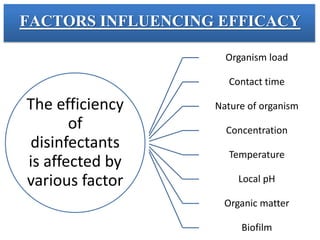
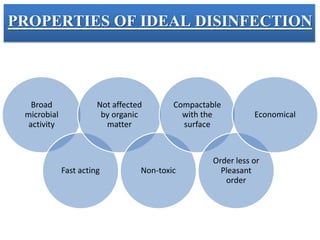
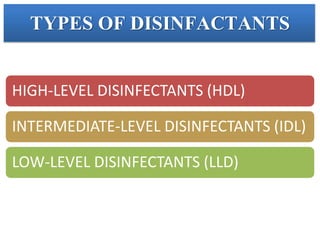
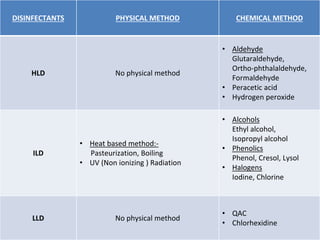
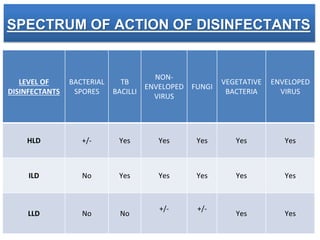
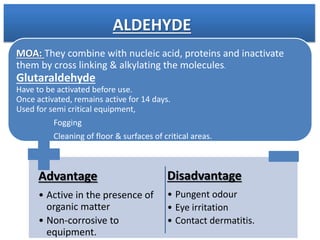
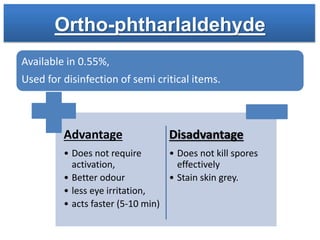
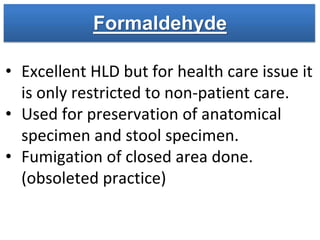
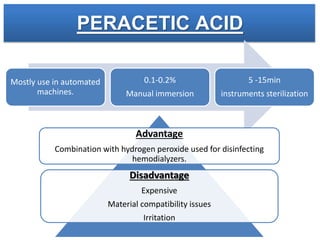
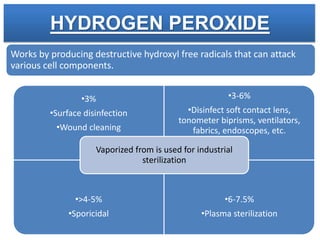
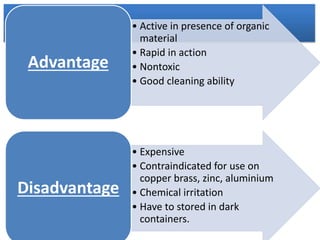
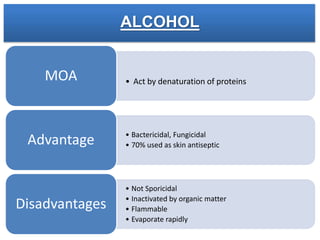
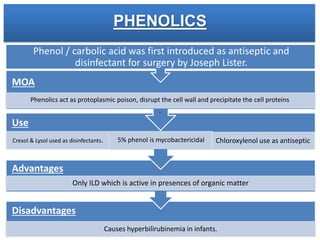
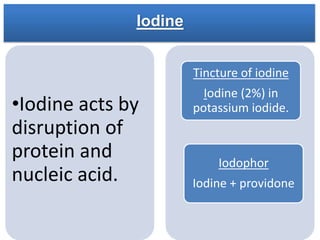
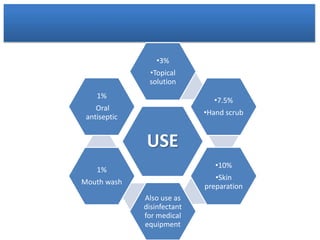
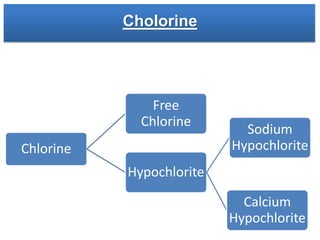
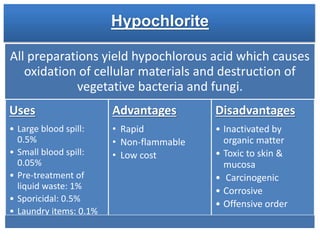
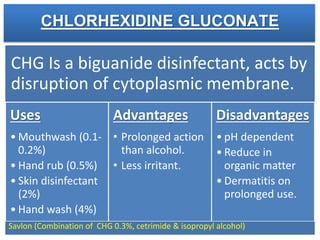
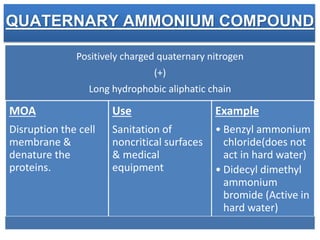
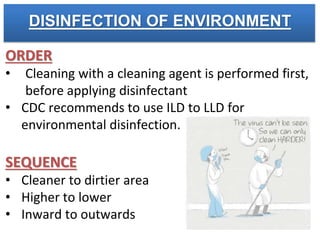
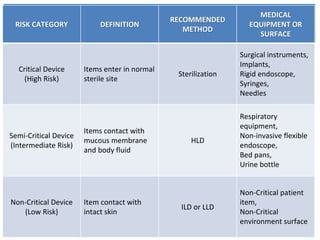
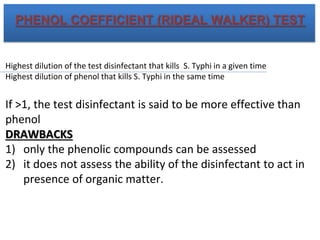
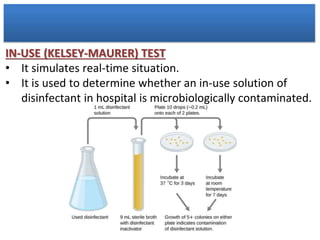
This document discusses various terms related to disinfection including sterilization, disinfection, sanitization, and asepsis. It describes factors that influence the efficacy of disinfectants such as organism load, contact time, and temperature. The document outlines the properties of ideal disinfection and types of disinfectants including high, intermediate, and low level disinfectants. Various chemical and physical disinfection methods are explained along with testing methods to evaluate disinfectant efficacy.