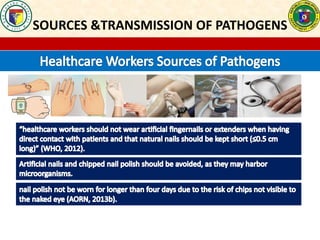
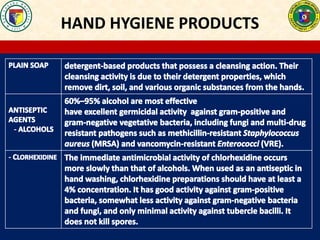
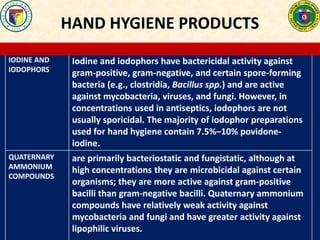
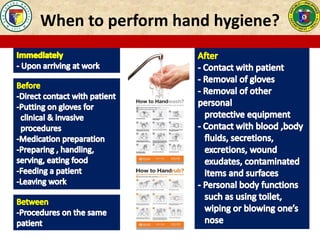
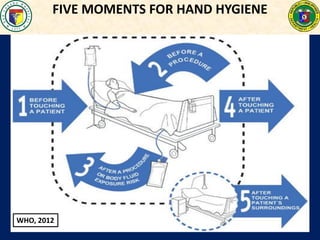
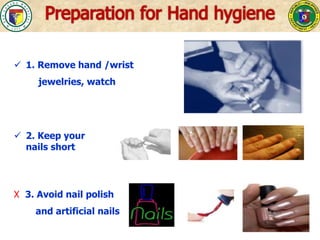
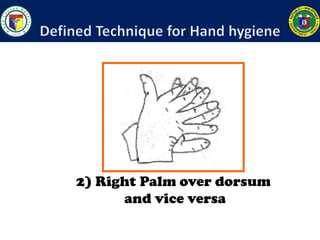
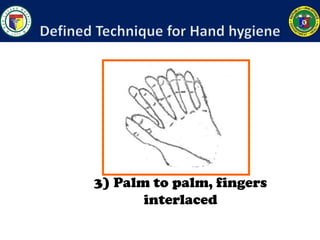
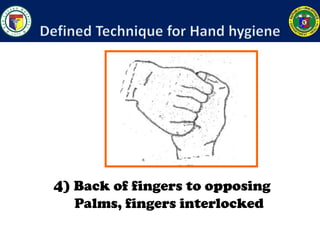
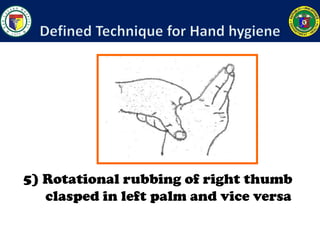
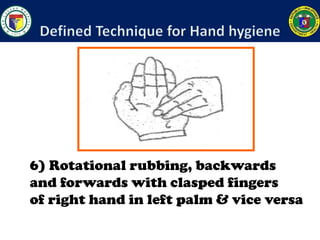
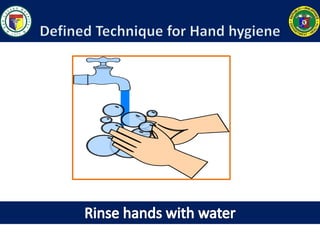
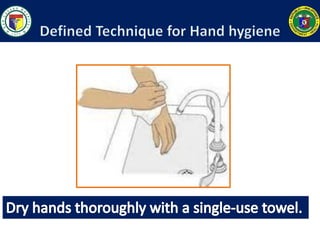
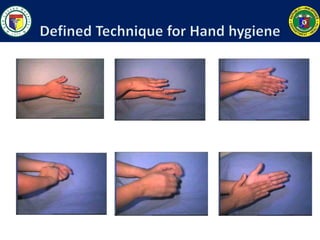
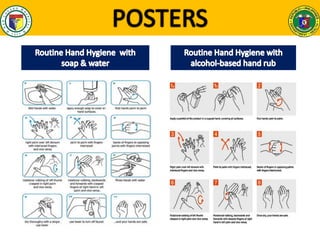
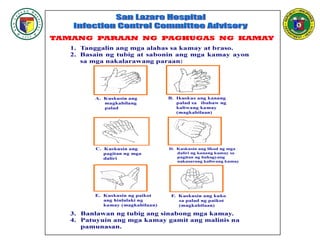
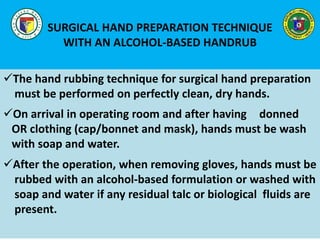
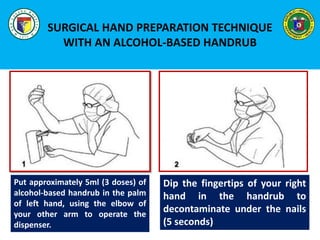
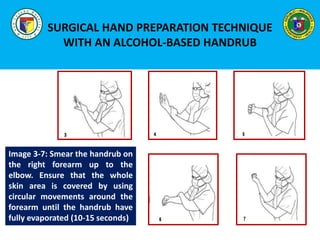
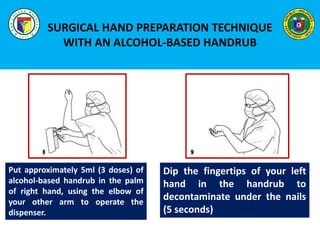
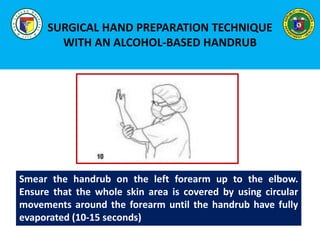
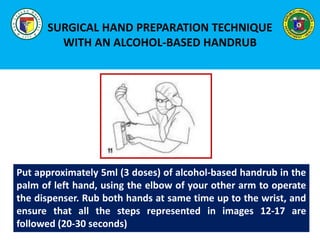
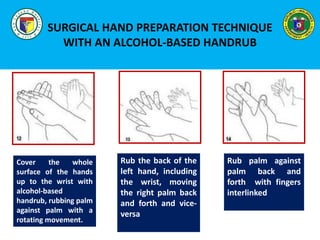
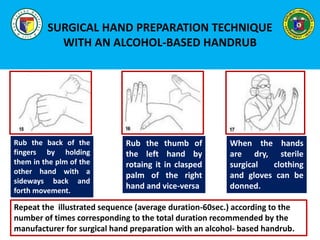
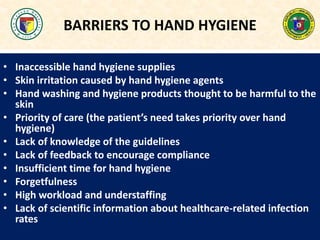
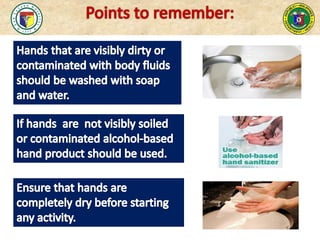
This document provides a history and overview of hand hygiene guidelines and practices in healthcare settings. It discusses how recommendations have evolved over time, from Semmelweis' work in 1846 demonstrating the importance of handwashing in reducing maternal mortality, to the WHO's 2009 guidelines recommending alcohol-based hand rubs when hands are not visibly soiled. The document outlines the five moments for hand hygiene according to WHO, reviews different hand hygiene products and techniques, including for surgical hand preparation, and discusses barriers to adherence and ways to promote a culture of hand hygiene compliance.