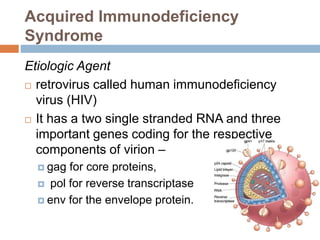
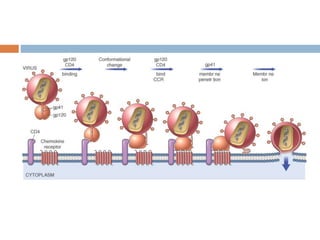
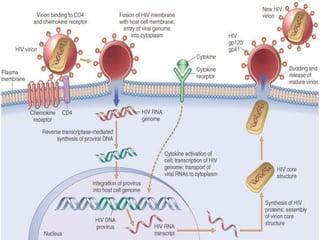
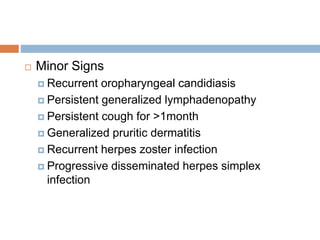
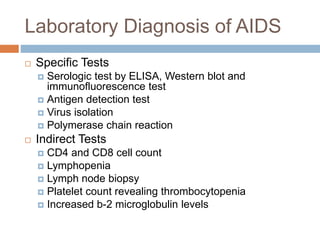
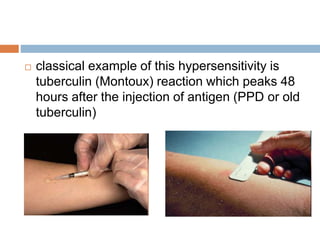
Immunity involves the body's resistance to pathogenic agents. It is broadly divided into innate and acquired immunity. Innate immunity is present from birth while acquired immunity develops after exposure to specific pathogens. Immunization helps prepare the body against diseases either through passive or active immunity. Immunodeficiency diseases are caused by inherited or secondary defects in immunity. Acquired Immunodeficiency Syndrome is caused by HIV and damages the immune system. Hypersensitivity reactions occur when the immune system overreacts to antigens and are classified into four types based on the mechanisms involved.