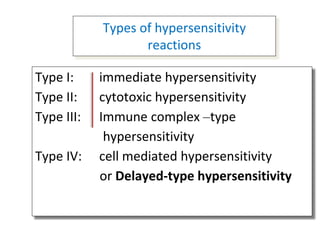
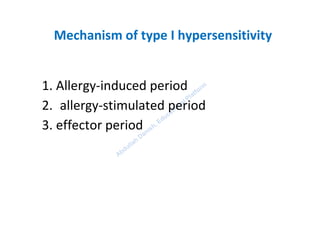
This document discusses different types of hypersensitivity reactions. It begins by defining hypersensitivity as an overreaction of the immune system to harmless antigens. It then describes the four main types of hypersensitivity reactions:
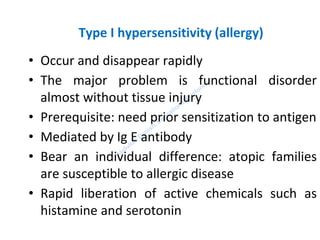
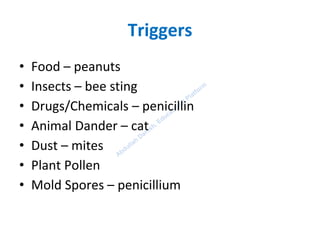
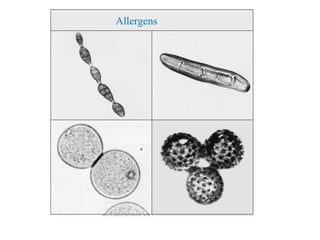
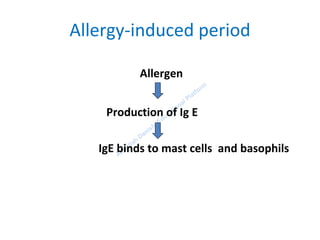
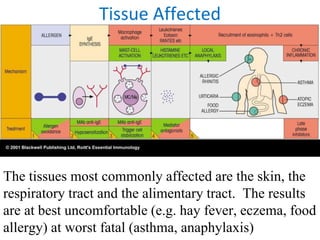
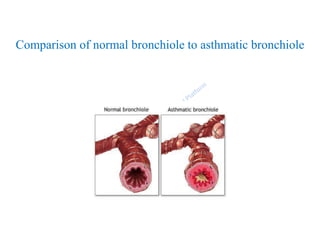
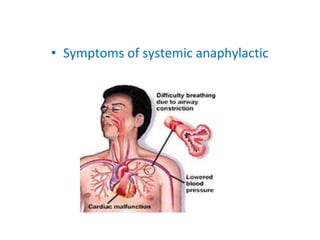
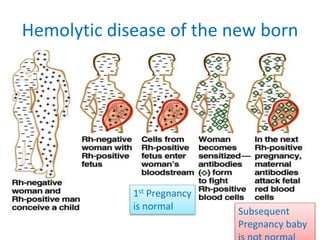
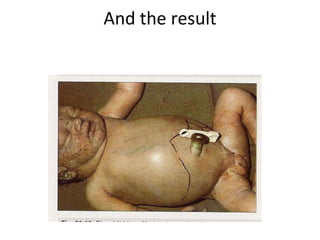
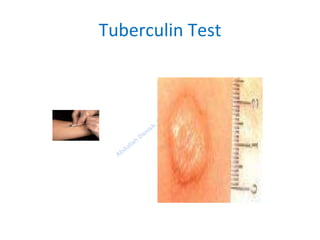
Type I is immediate hypersensitivity mediated by IgE antibodies, commonly seen in allergies. Type II involves IgG/IgM antibodies attacking self cells, seen in hemolytic disease of newborns. Type III occurs when immune complexes deposit in tissues, causing conditions like serum sickness. Type IV is cell-mediated/delayed hypersensitivity exemplified by the Mantoux tuberculin skin test reaction.