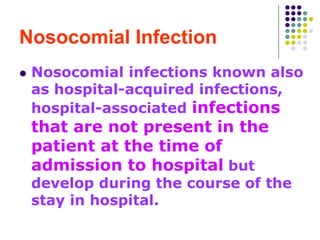
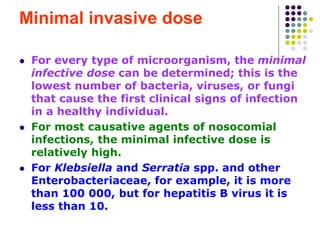
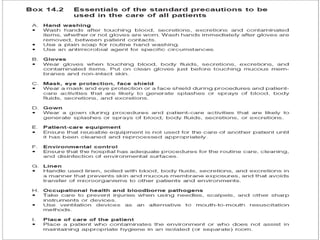
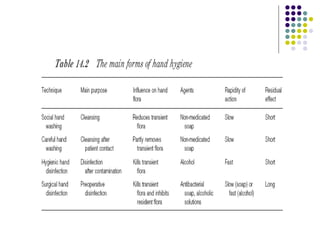
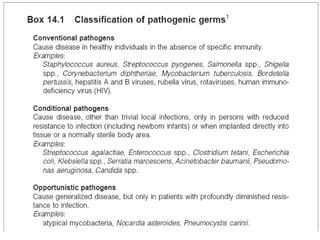
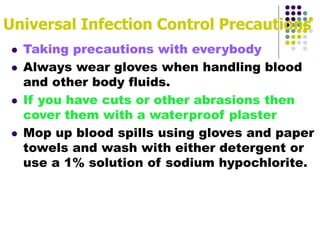
This document discusses nosocomial (hospital-acquired) infections. It defines nosocomial infections as those not present in a patient upon admission but develop during their hospital stay. It describes the different types of nosocomial infections including endogenous and cross-contamination. Key factors that contribute to the spread of nosocomial infections are discussed such as normal flora, carriers, routes of transmission including direct/indirect contact and airborne, and prevention methods like isolation, cleaning, sterilization, and hand hygiene. Universal precautions are also summarized as important to prevent the transmission of infections.