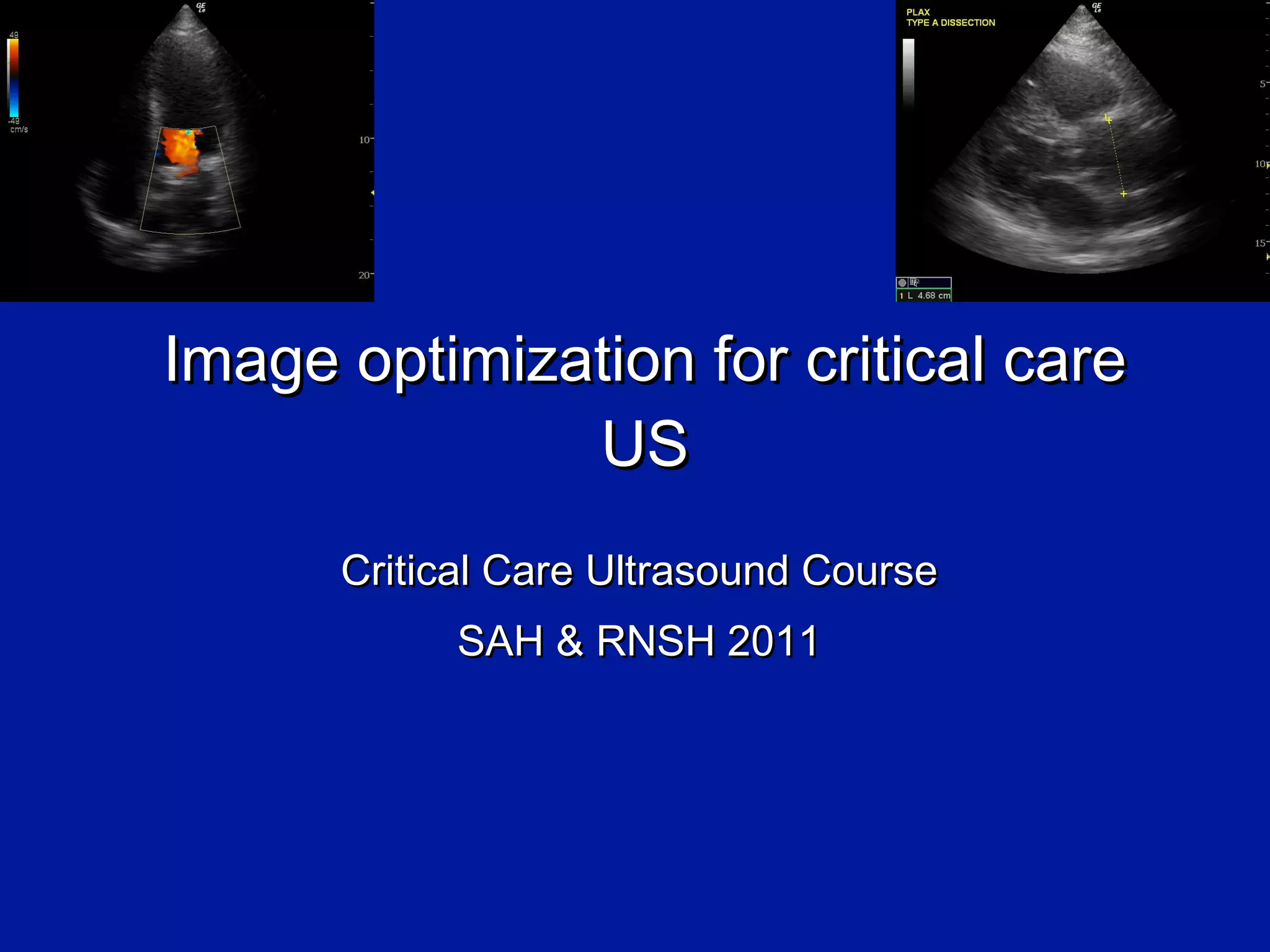
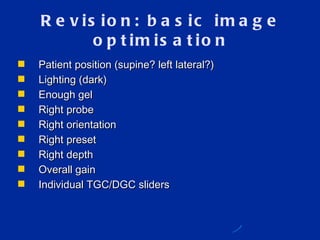
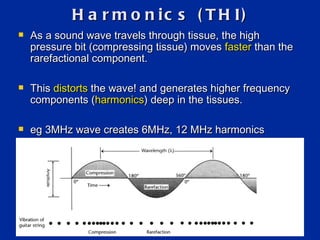
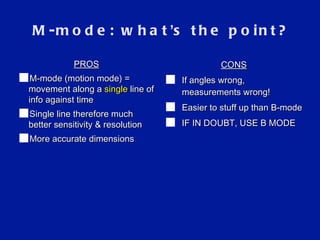
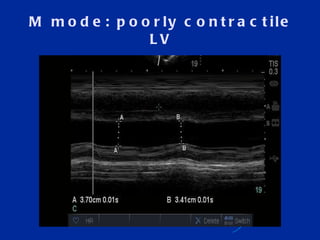
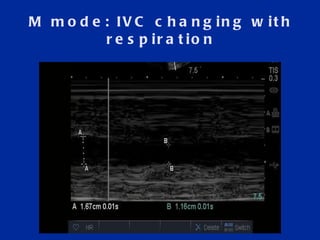
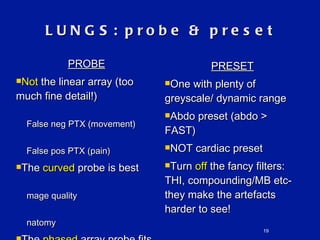
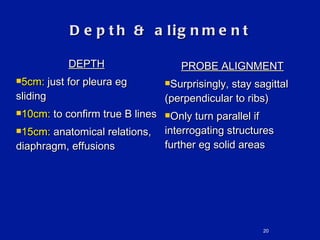
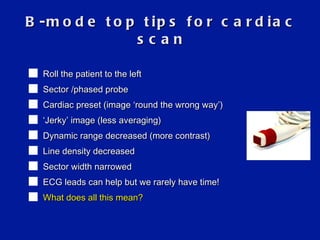
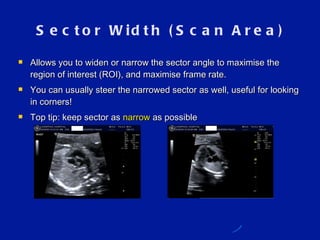
This document provides guidance on optimizing ultrasound images for critical care applications. It discusses adjusting various image settings like depth, focal zones, harmonics and M-mode to improve image quality for assessing lungs, IVC, and heart. M-mode is recommended for measuring movement and dimensions more accurately than B-mode. The challenges of cardiac imaging are also covered, noting the need for higher frame rates and reduced averaging and spatial resolution to capture fast heart motion. Narrowing the sector width and decreasing depth can help optimize the cardiac image within these limits.