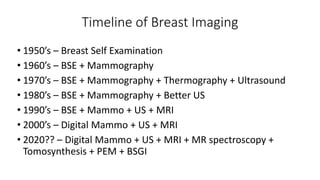
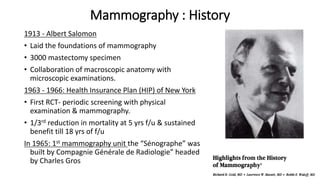
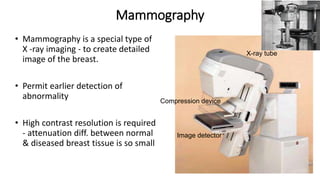
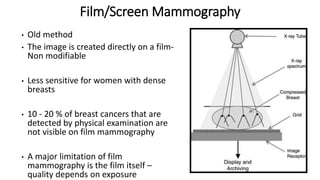
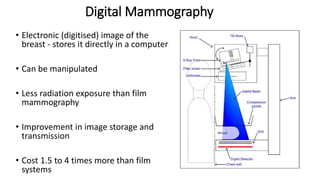
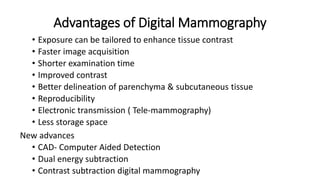
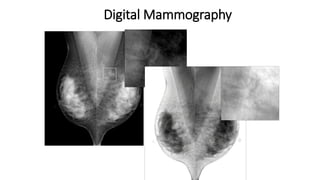
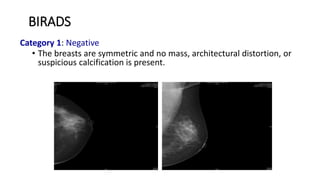
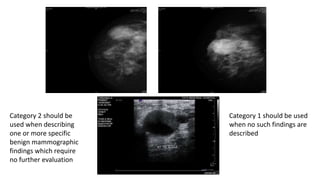
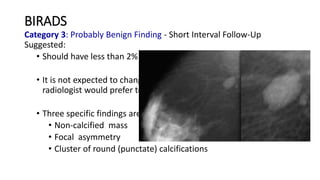
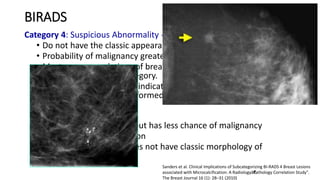
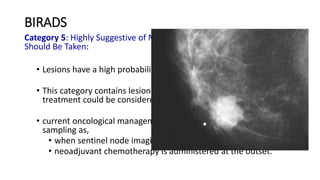
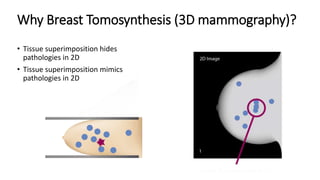
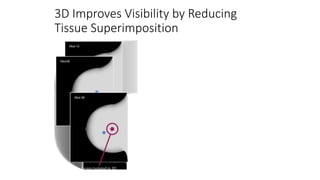
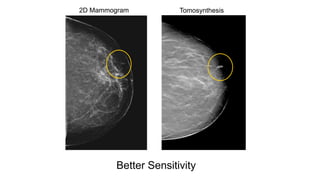
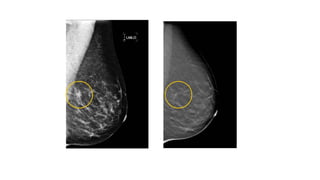
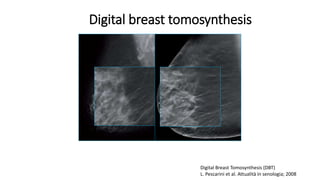
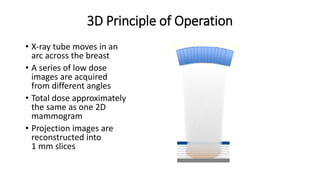
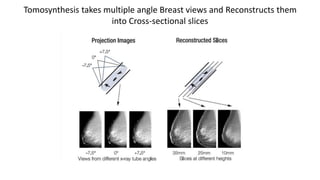
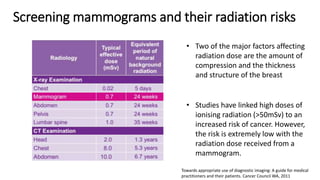
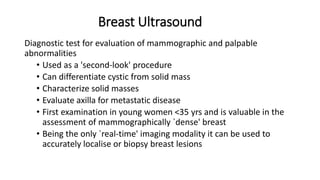
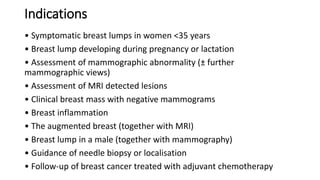
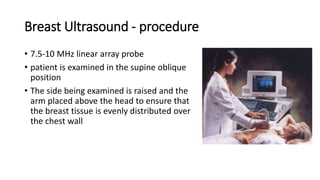
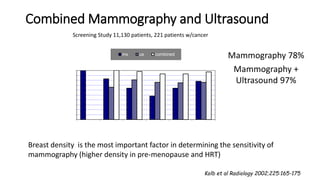
Breast imaging techniques have advanced significantly since the 1950s. Mammography was introduced in the 1960s and digital mammography in the 2000s improved image quality and reduced radiation exposure. Tomosynthesis was developed in the 2010s to reduce tissue superimposition by creating 1mm slices. Ultrasound is used as an adjunct to mammography to differentiate cysts from solid masses and guide biopsies. The BI-RADS classification system standardizes how breast imaging findings are reported and communicated. While mammography remains the primary breast cancer screening tool, tomosynthesis and ultrasound have improved cancer detection rates by reducing false negatives, especially for women with dense breasts.