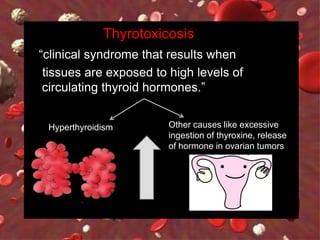
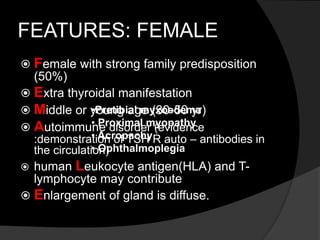
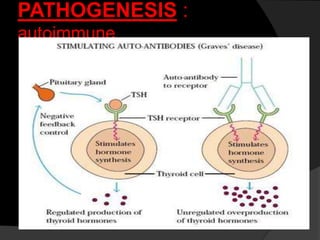
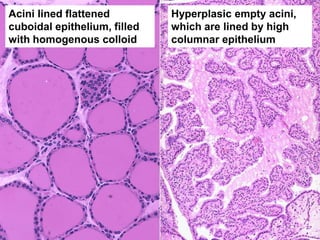
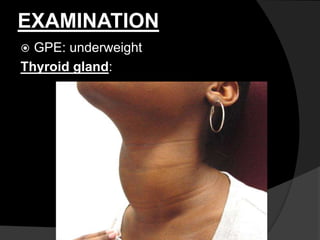
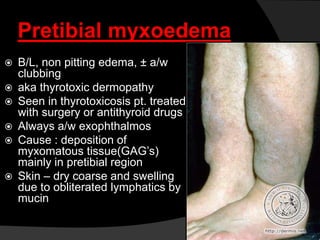
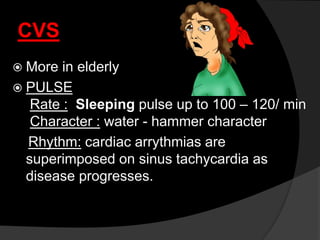
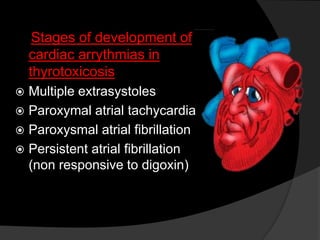
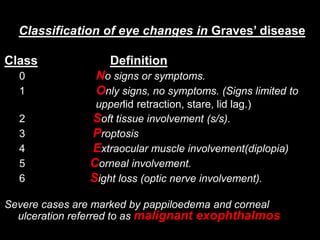
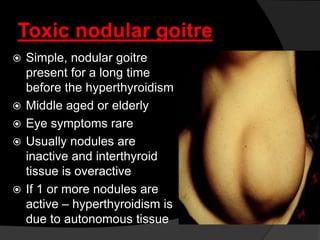
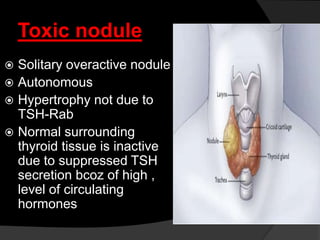
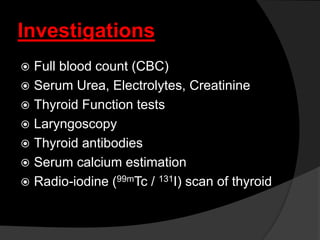
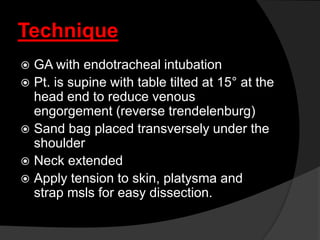
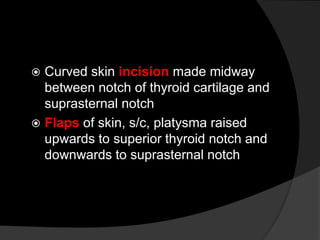
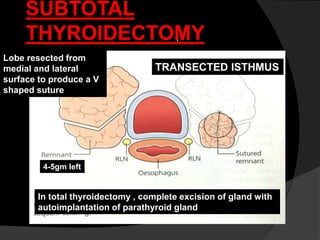
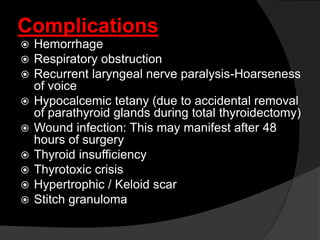
Thyrotoxicosis is a clinical syndrome caused by high levels of circulating thyroid hormones, with primary causes including Graves' disease and toxic nodular goiter, leading to symptoms of weight loss, fatigue, heat intolerance, and emotional changes. Diagnosis is based on examination findings of a goiter, tachycardia, and eye changes like exophthalmos, with treatment options including antithyroid drugs, radioactive iodine, or surgery to remove the overactive thyroid tissue.