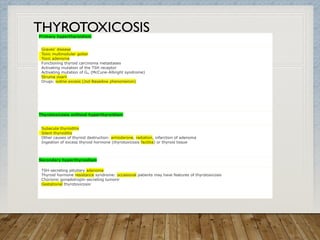
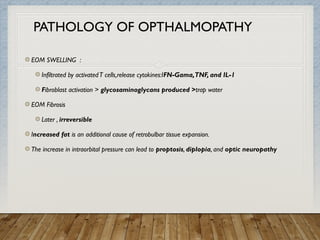
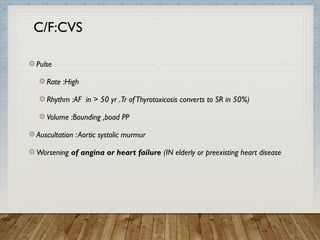
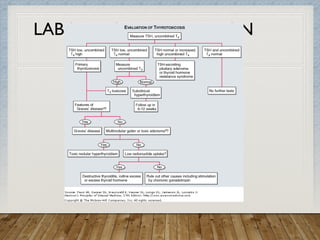
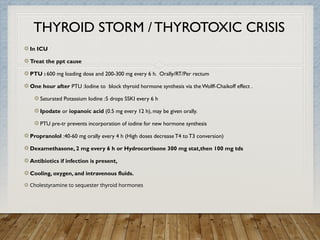
The document provides a comprehensive overview of hyperthyroidism, particularly focusing on Graves' disease as a major cause of thyrotoxicosis, including its pathogenesis, clinical features, diagnostics, and treatment options. It discusses the incidence, clinical signs and symptoms, ophthalmopathy associated with Graves', complications, and various treatment strategies such as antithyroid drugs, radioiodine, and surgery. Additional information is provided on the management of thyroid-related conditions during pregnancy and thyroid storm, as well as various other potential causes of thyrotoxicosis.