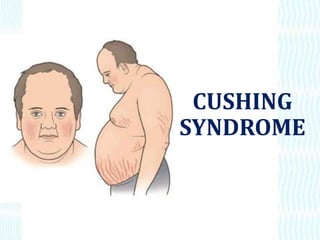
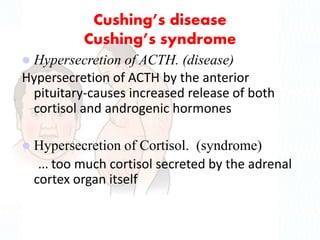
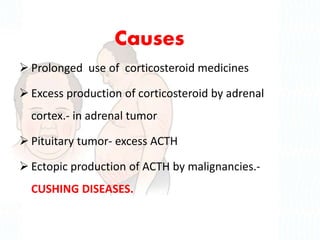
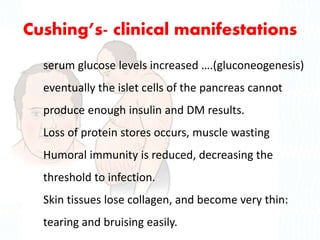
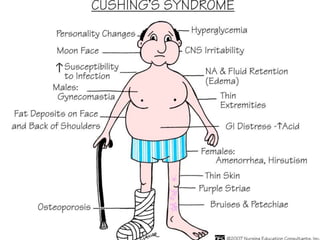
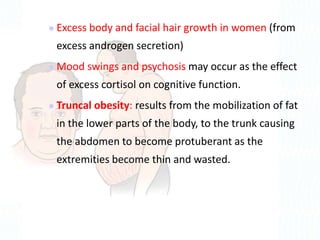
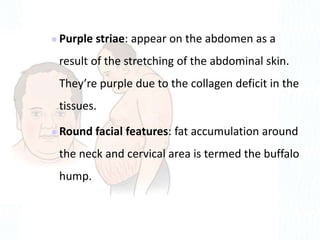
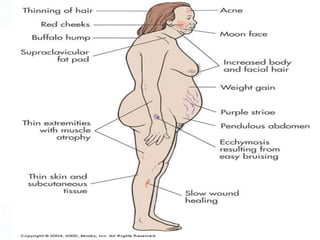
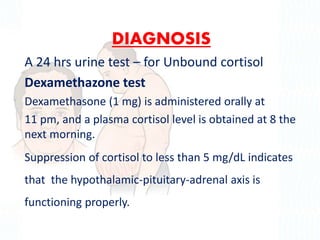
Cushing syndrome is characterized by excess cortisol secretion caused by too much ACTH from the pituitary gland or excess cortisol from adrenal tumors. It presents with weight gain, thin extremities, moon face, skin changes, and metabolic complications. Diagnosis involves urine and blood tests to measure cortisol levels. Treatment depends on the underlying cause but may include surgery to remove tumors, radiation therapy, or medications to reduce cortisol levels. Nursing care focuses on preventing infections, injuries, skin breakdown and improving nutrition, fluid balance and body image.