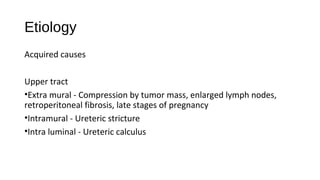
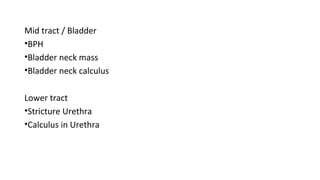
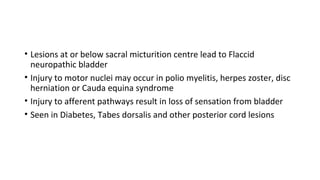
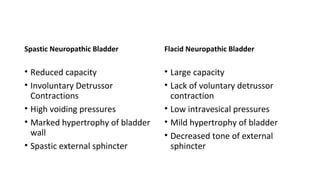
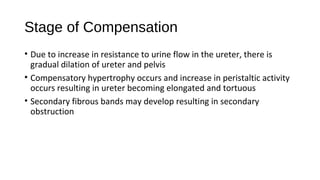
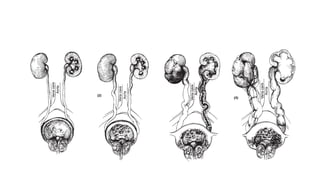
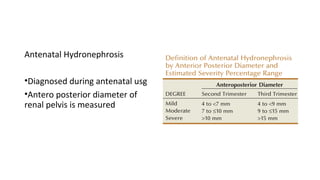
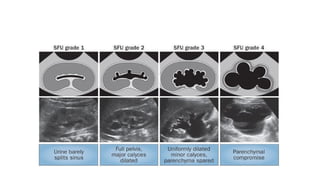
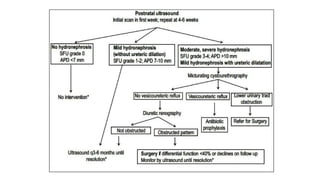
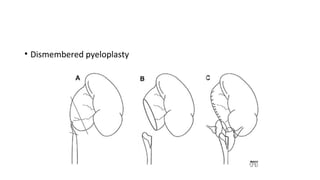
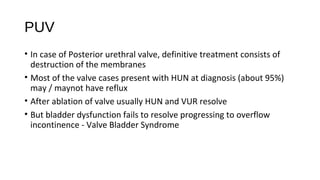
This document provides an overview of hydronephrosis, including definitions, etiology, pathophysiology, clinical features, investigations, and management. Hydronephrosis is dilation of the renal pelvis or calyces that can be associated with obstruction. The causes include congenital issues like PUJ obstruction or acquired issues like ureteral strictures. Untreated obstruction can lead to renal damage through stages of compensation and decompensation. Clinical features depend on the cause but may include loin or groin pain. Investigations include imaging like ultrasound, IVU, CT scan, and urodynamics. Management involves relieving obstruction through surgery or stenting as well as treating infections.