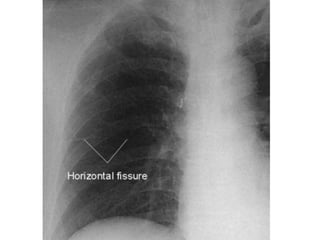
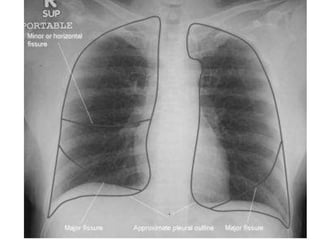
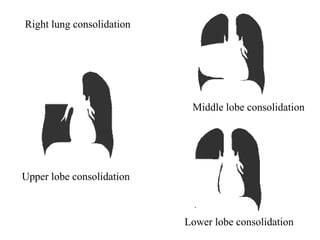
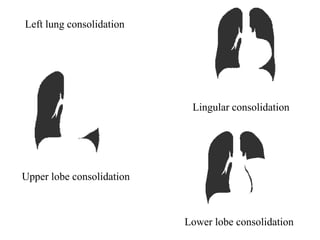
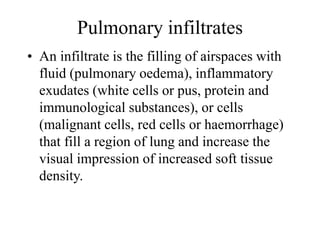
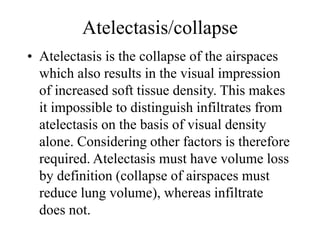
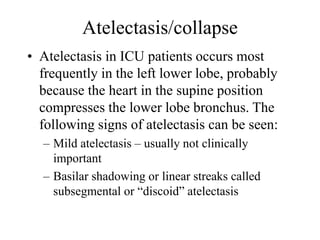
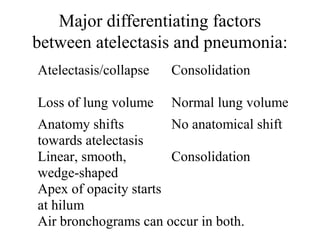
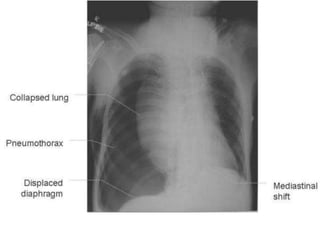
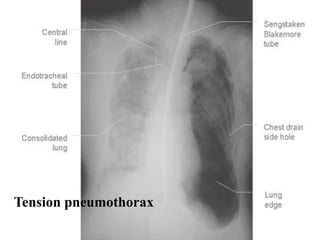
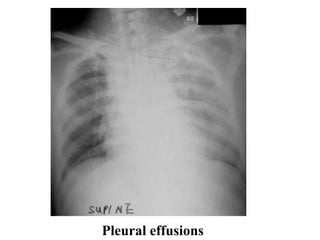
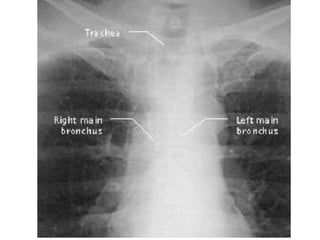
1. The document describes various lung abnormalities that can be seen on chest x-rays including pneumonia, pulmonary edema, atelectasis, consolidation, and pneumothorax.
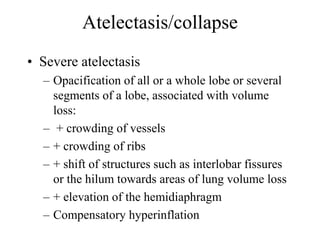
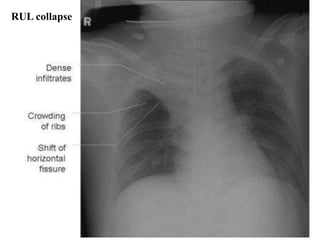
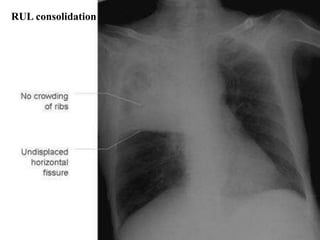
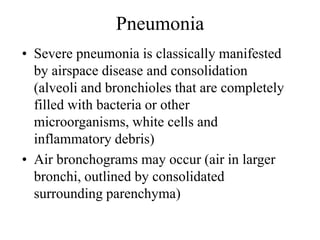
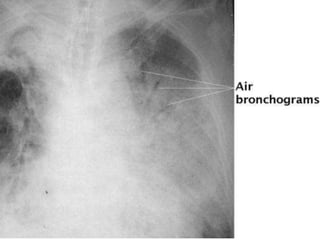
2. Characteristics of different pathologies are outlined such as signs of atelectasis including crowding of vessels and volume loss. Pneumonia is described as airspace disease and consolidation with possible air bronchograms.
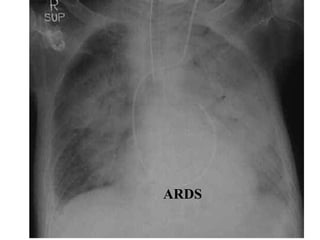
3. Pulmonary edema, ARDS, and other conditions are also briefly summarized with mentions of typical radiographic findings like Kerley lines for pulmonary edema.