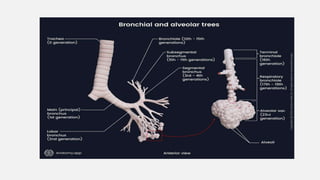
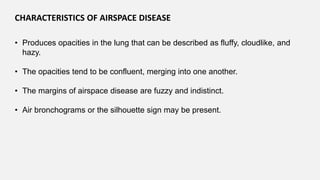
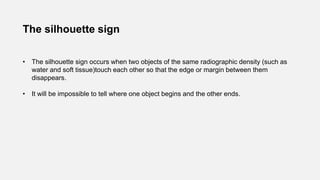
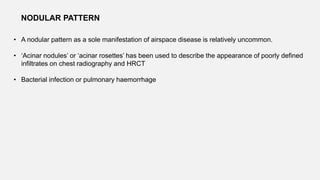
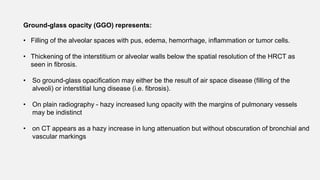
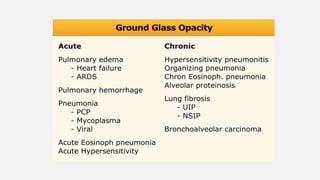
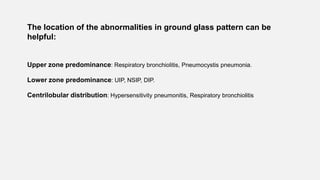
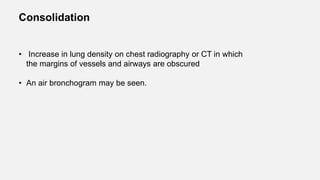
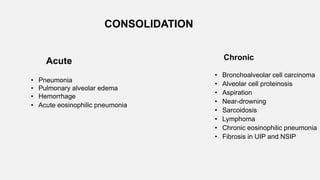
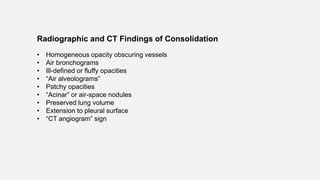
This document discusses air space diseases, which are pathological processes that displace air from the alveoli. Air spaces can be filled with fluid, pus, blood or cells. Characteristics of air space disease include fluffy, cloudlike opacities that are confluent and have fuzzy margins. Common signs are air bronchograms and the silhouette sign. Different patterns include nodular, ground glass opacification and consolidation. The causes and differential diagnosis of each pattern are described based on location, time course and appearance.








![• Pathologic processes can result in air-space
consolidation:
1. Water (e.g., the various types of pulmonary edema)
2. Blood (e.g., pulmonary hemorrhage)
3. Pus (e.g., pneumonia)
4. Cells (e.g., pulmonary adenocarcinoma, lymphoma, eosinophilic
pneumonia, organizing
pneumonia [OP])
5. Other substances (e.g., lipoprotein in alveolar proteinosis, lipid in lipoid
pneumonia](https://image.slidesharecdn.com/airspace1-220815092018-8282090d/85/Air-Space-Diseases-pptx-17-320.jpg)



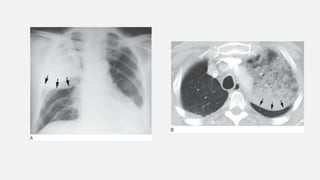
![Perihilar “Bat-Wing” Consolidation
Shows central consolidation with sparing of the lung periphery
Pulmonary edema
This pattern also may be seen with:
• pulmonary hemorrhage
• pneumonias
(including bacteria and atypical pneumonias such as Pneumocystis jiroveci pneumonia
[PCP]
and viral pneumonia)
• inhalational lung injury.](https://image.slidesharecdn.com/airspace1-220815092018-8282090d/85/Air-Space-Diseases-pptx-25-320.jpg)



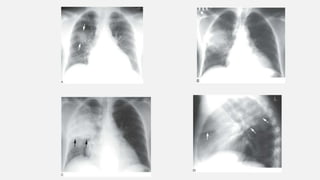
![Diffuse Air-space Nodules
This appearance is seen in patients with endobronchial spread
of infection such as :
• Tuberculosis (TB) or Mycobacterium avium complex (MAC) bacterial
• bronchopneumonia
• viral pneumonia (cytomegalovirus [CMV], measles)
• invasive mucinous adenocarcinoma with endobronchial spread
• pulmonary hemorrhage
• aspiration.](https://image.slidesharecdn.com/airspace1-220815092018-8282090d/85/Air-Space-Diseases-pptx-31-320.jpg)