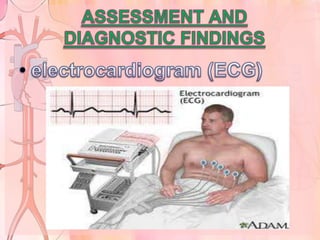
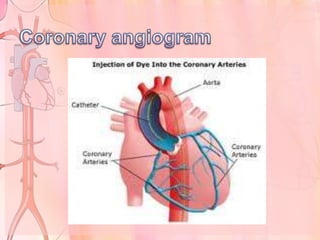
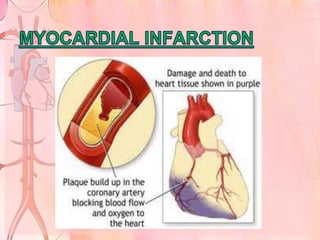
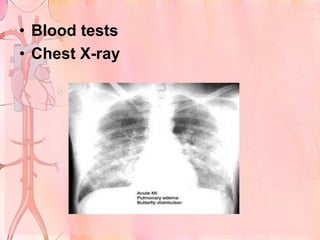
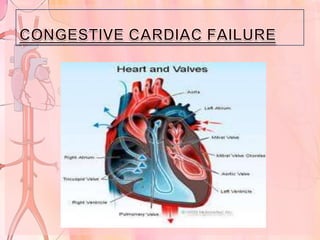
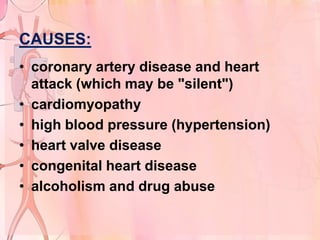
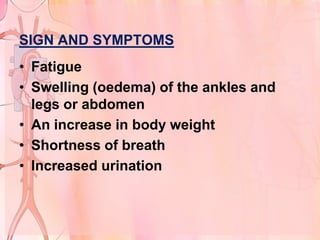
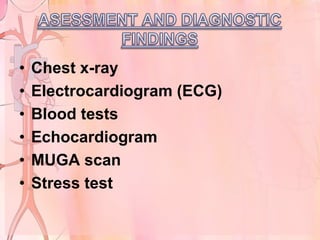
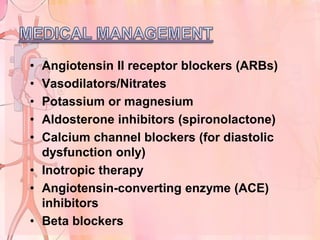
This document discusses cardiac emergencies including angina pectoris, myocardial infarction, and congestive cardiac failure. It defines each condition, lists causes and risk factors, describes signs and symptoms, outlines diagnostic tests and treatment options, discusses complications, and provides nursing management guidelines. Angina is chest pain due to decreased blood flow to the heart while myocardial infarction and congestive cardiac failure involve the heart's inability to pump sufficiently due to disease or damage. Prompt recognition and treatment are important to save lives during these deadly emergencies.