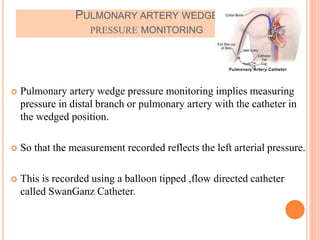
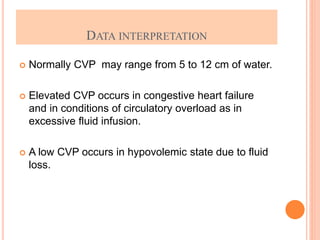
This document discusses hemodynamic monitoring, which refers to measuring the pressure, flow, and oxygenation of blood within the cardiovascular system. It describes various hemodynamic monitoring techniques like arterial blood pressure monitoring, pulmonary artery wedge pressure monitoring, and central venous pressure measurement. The purposes, principles, indications, and potential complications of these techniques are explained. Nurses have important responsibilities like preventing air embolism, clot formation, and fluid overload when patients receive hemodynamic monitoring.























![Clinicalteaching [autosaved]](https://image.slidesharecdn.com/clinicalteachingautosaved-180718063103/85/Clinicalteaching-autosaved-29-320.jpg)