Embed presentation
Downloaded 21 times
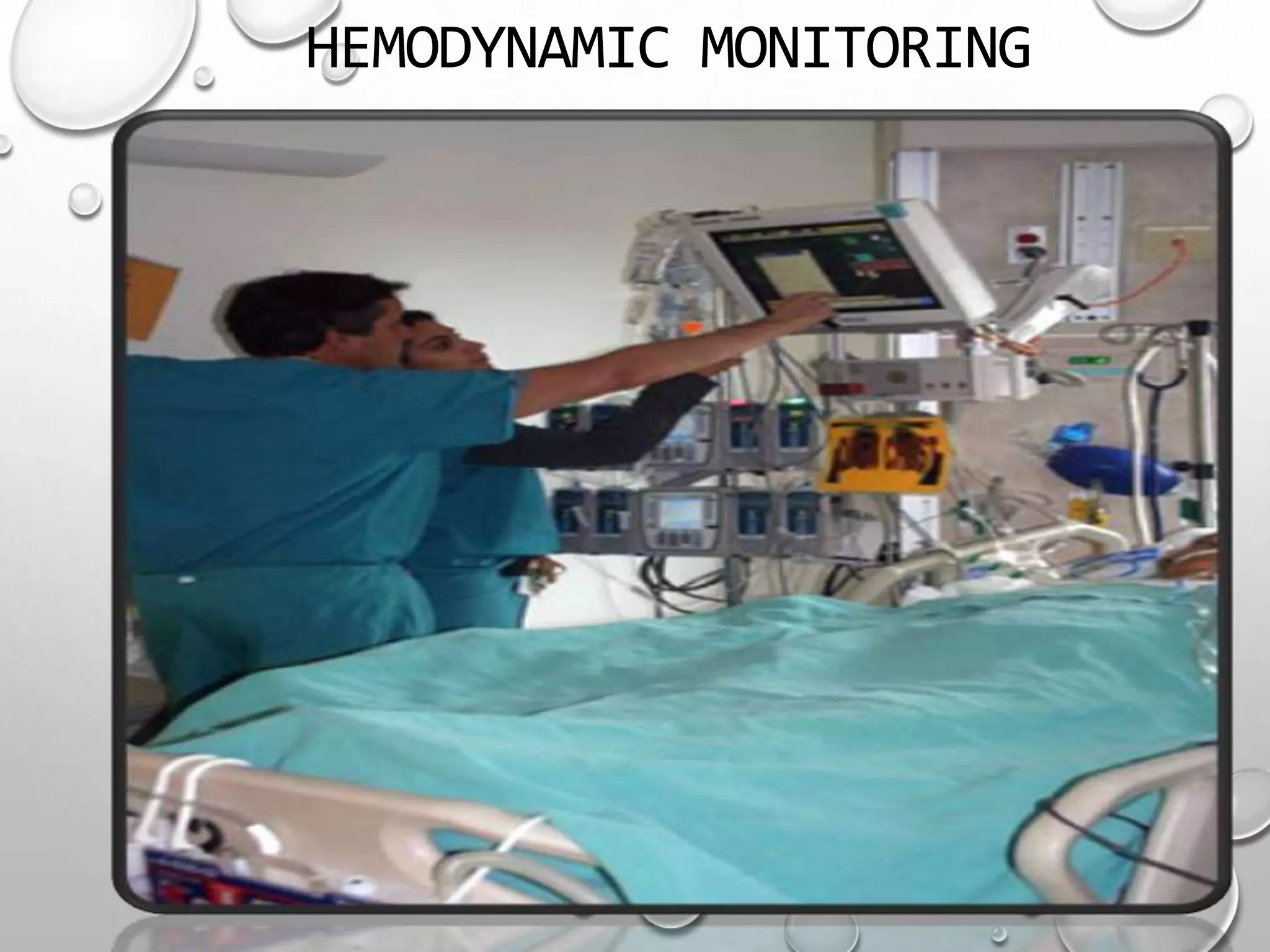
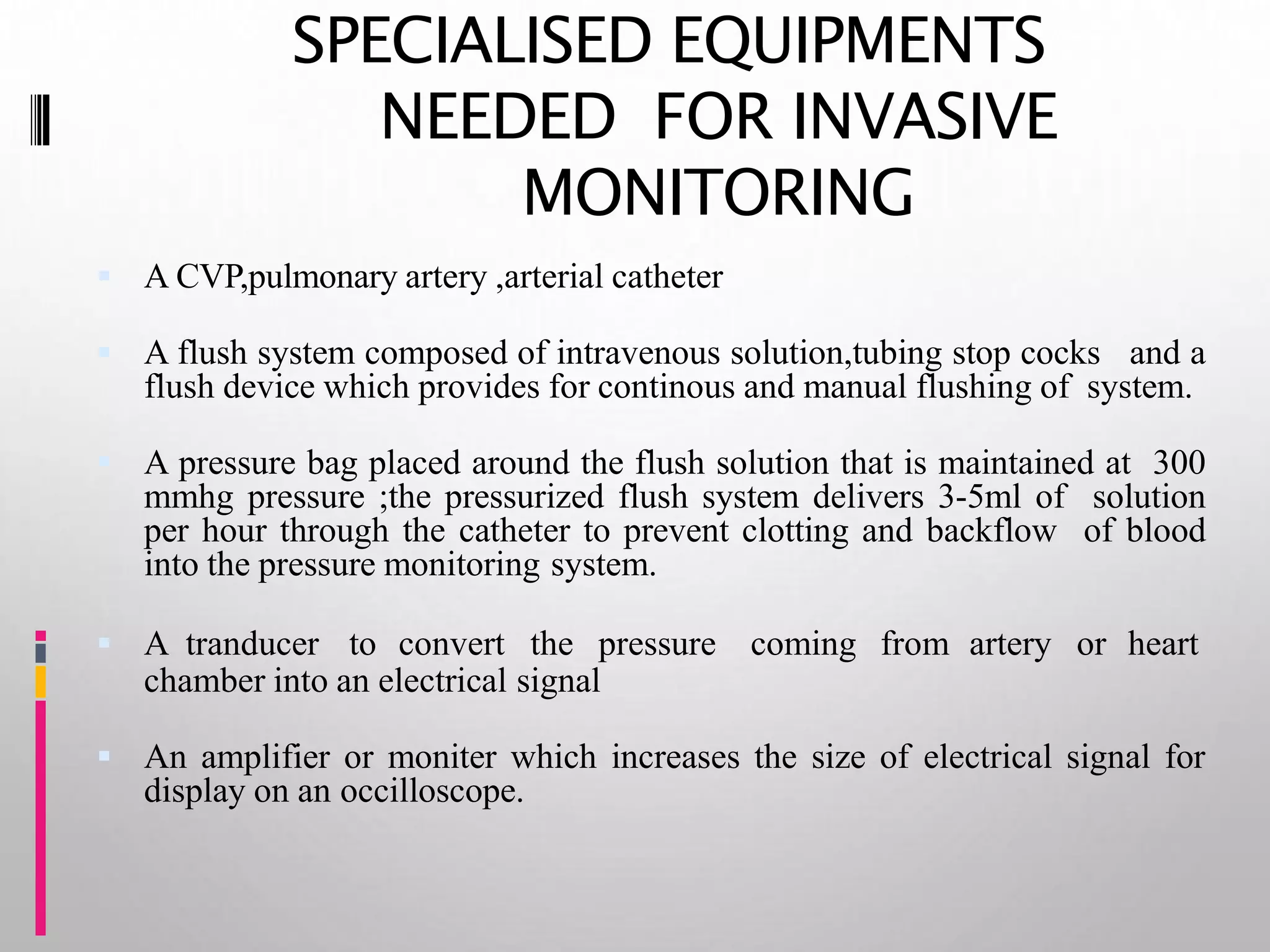
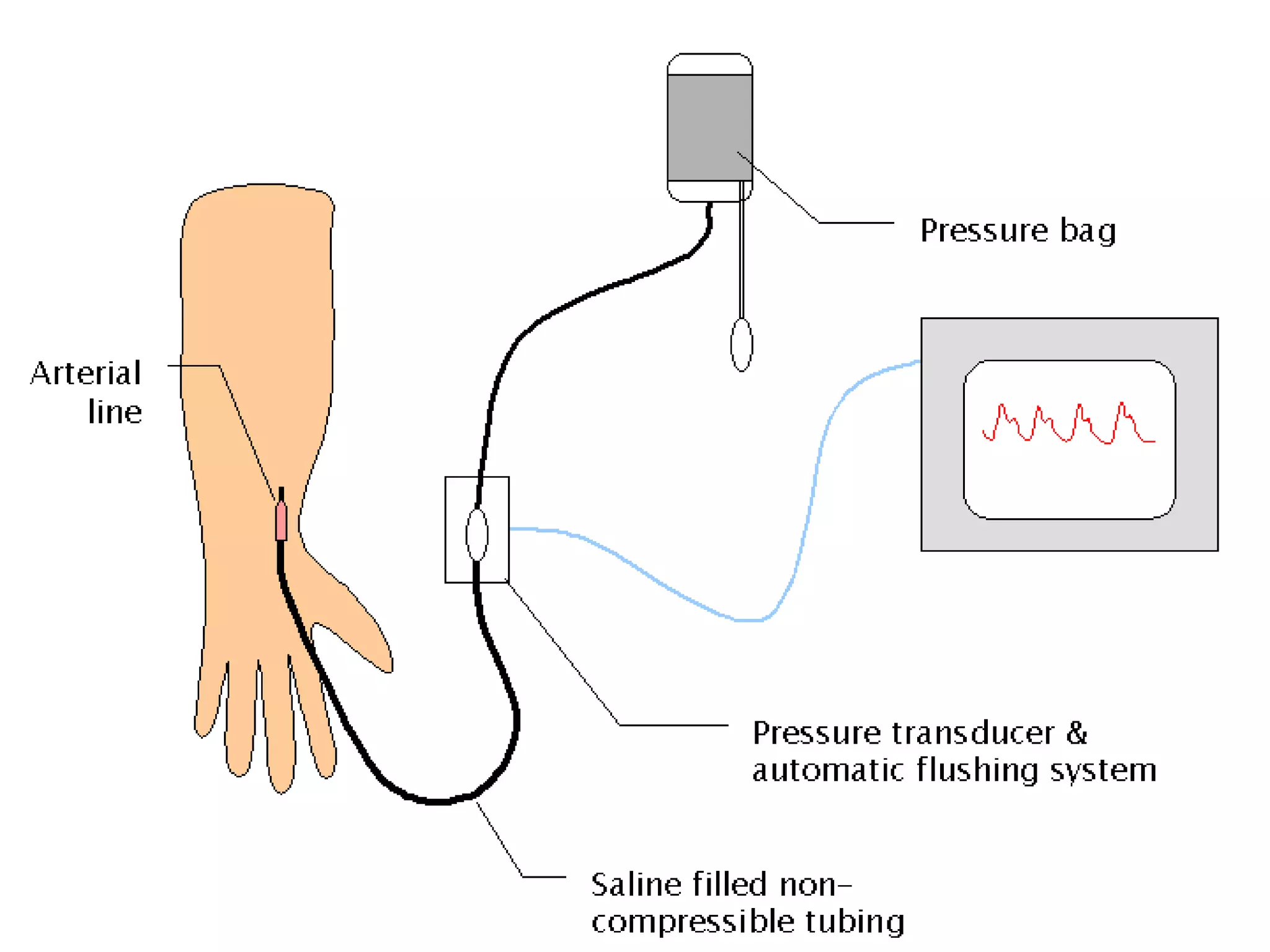
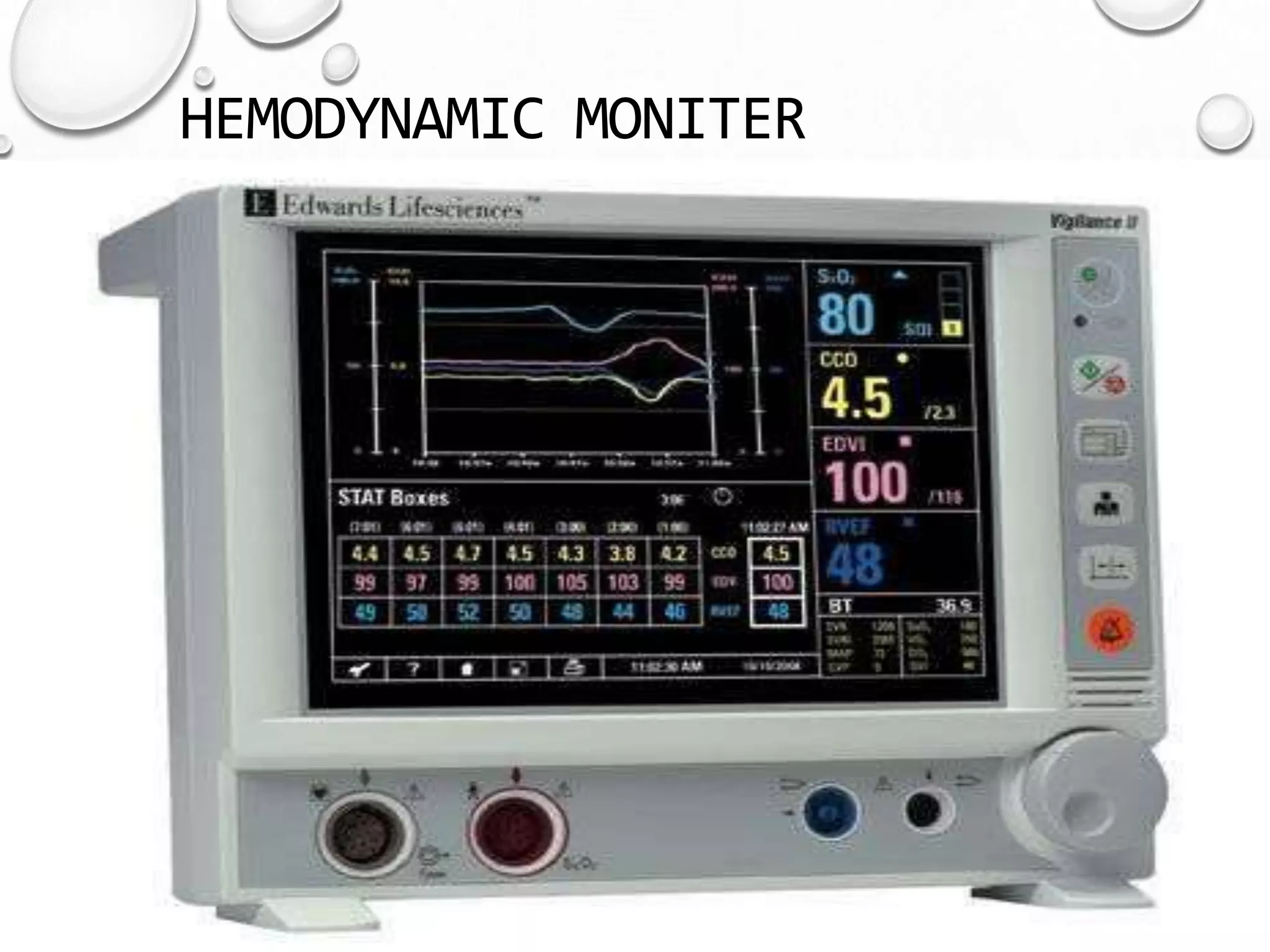
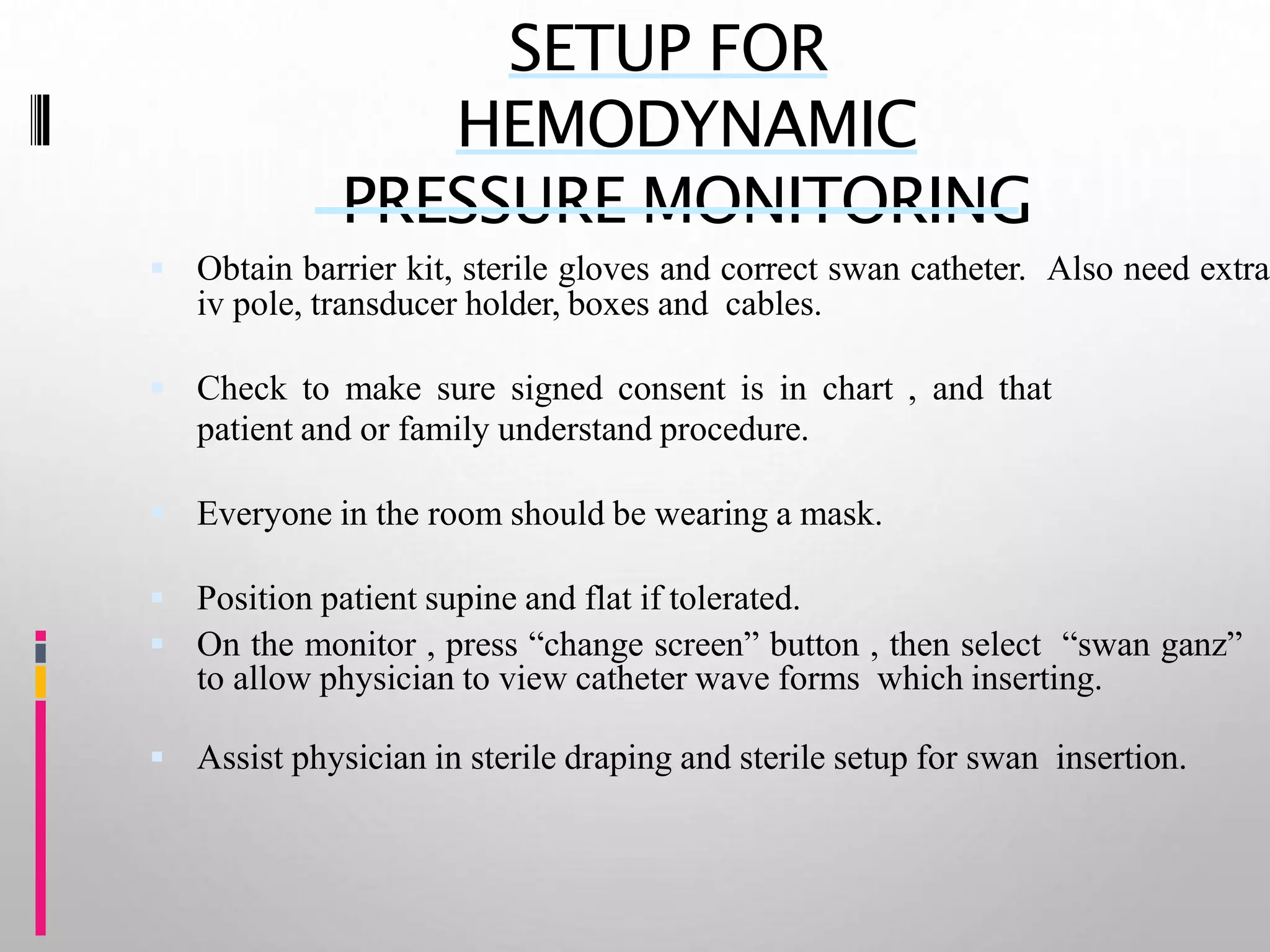
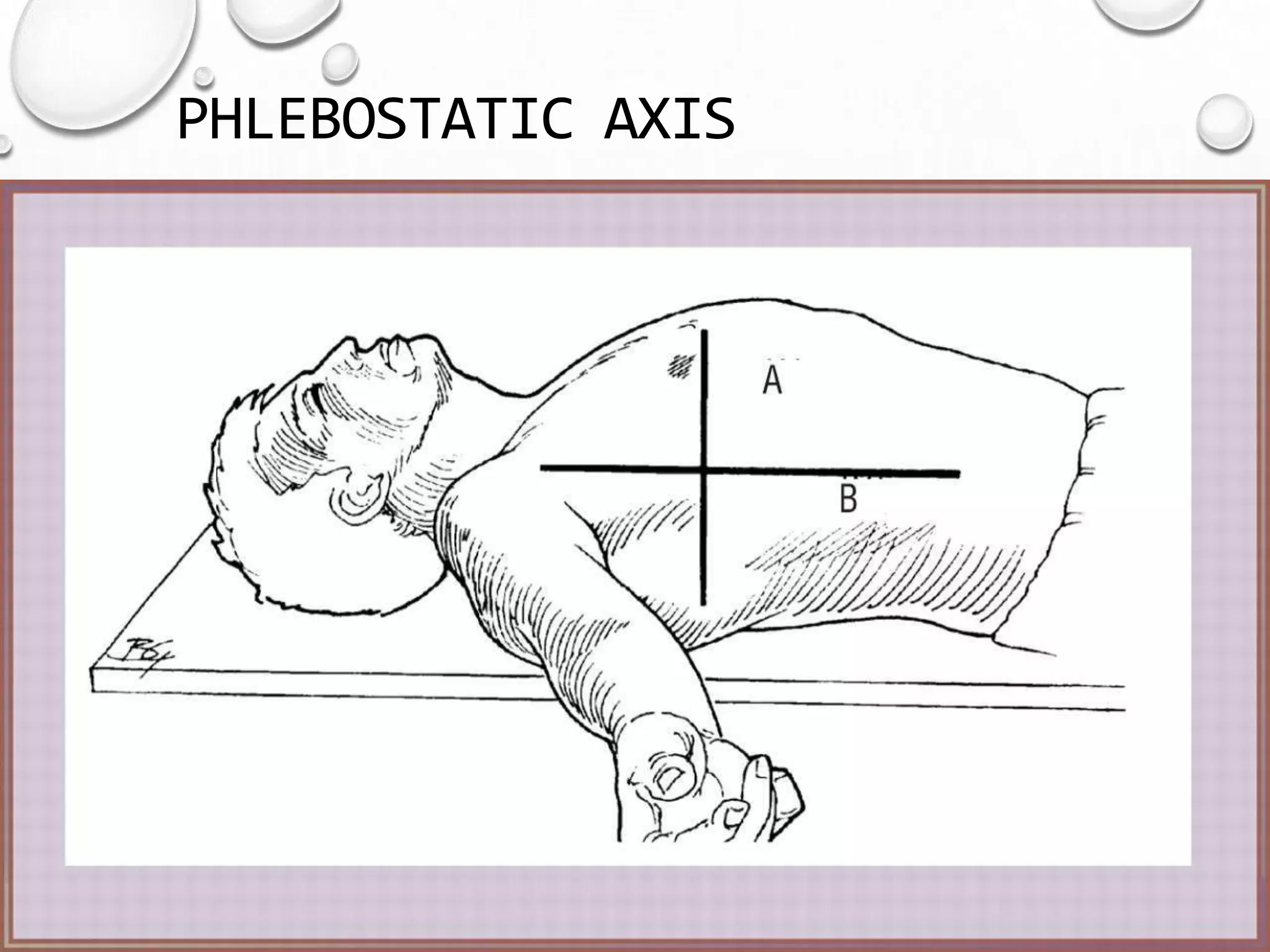
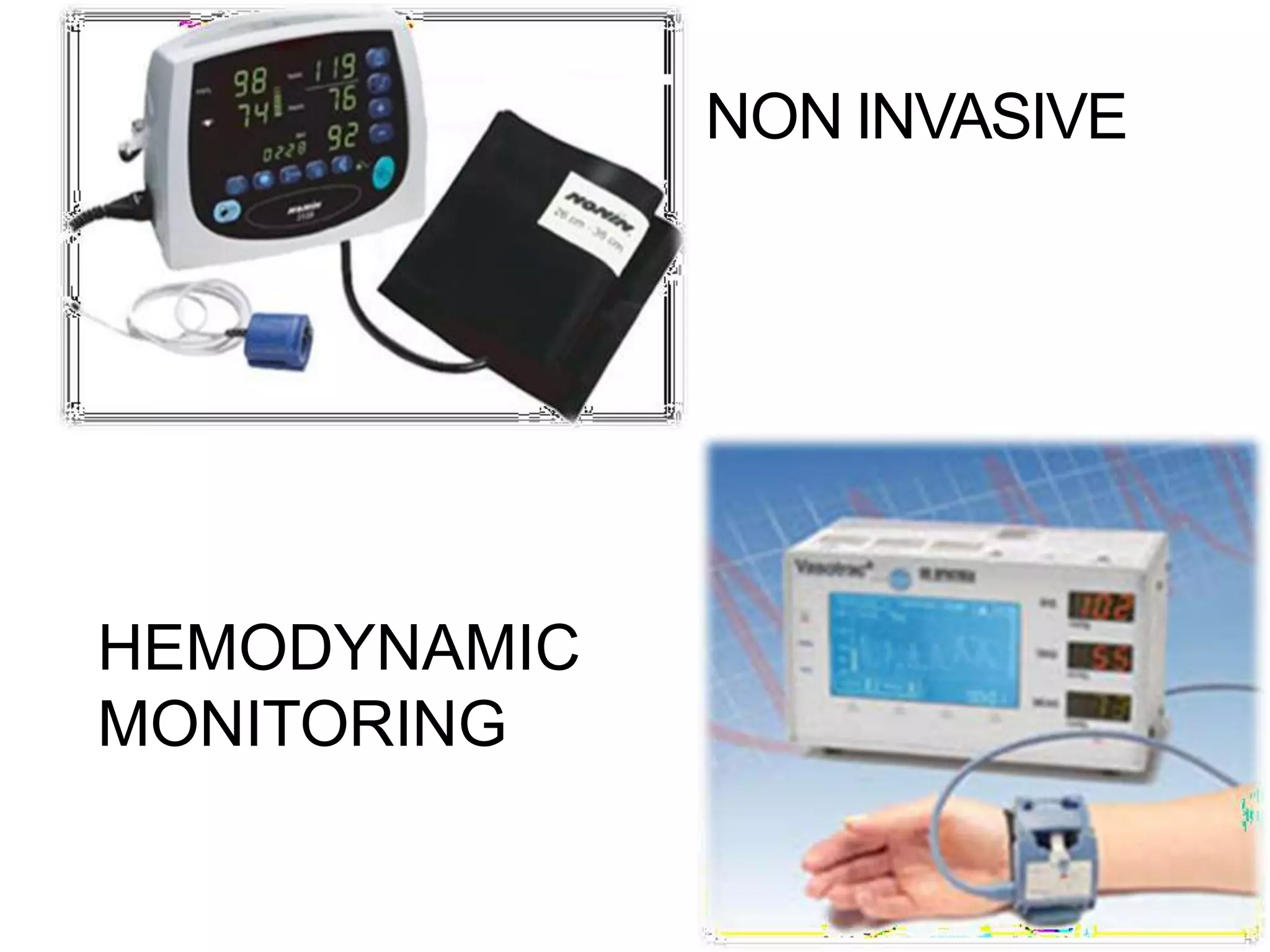
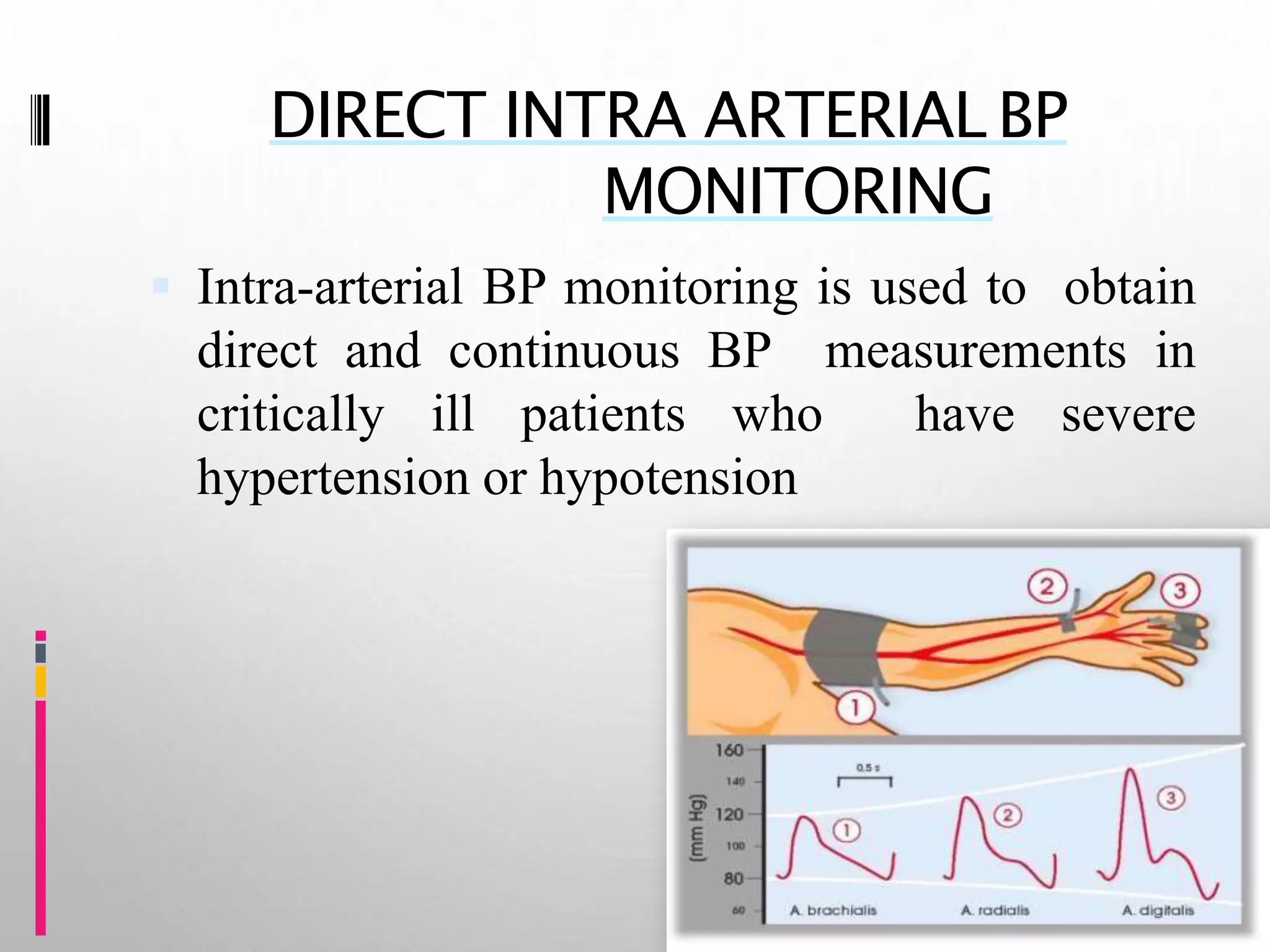
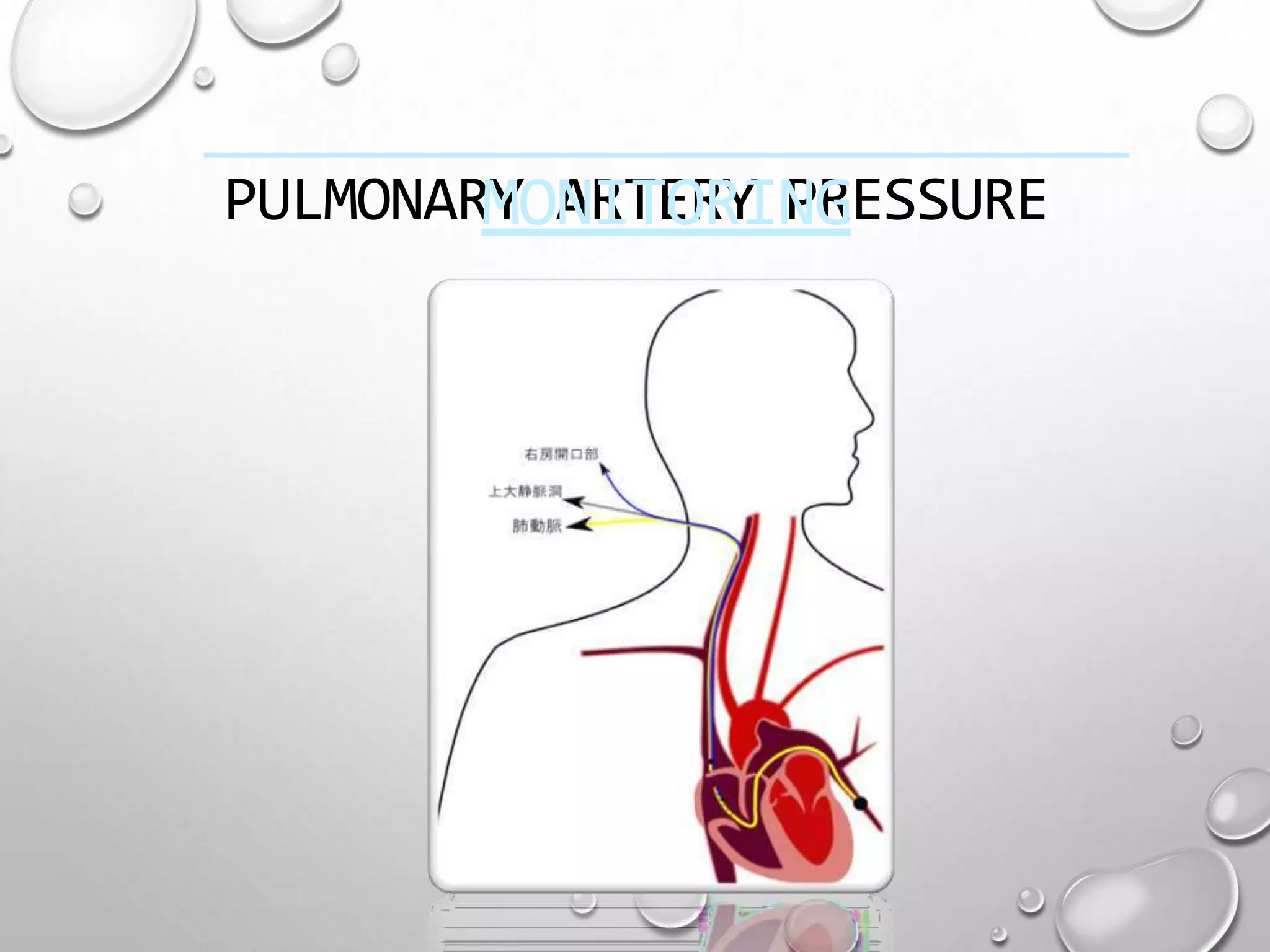
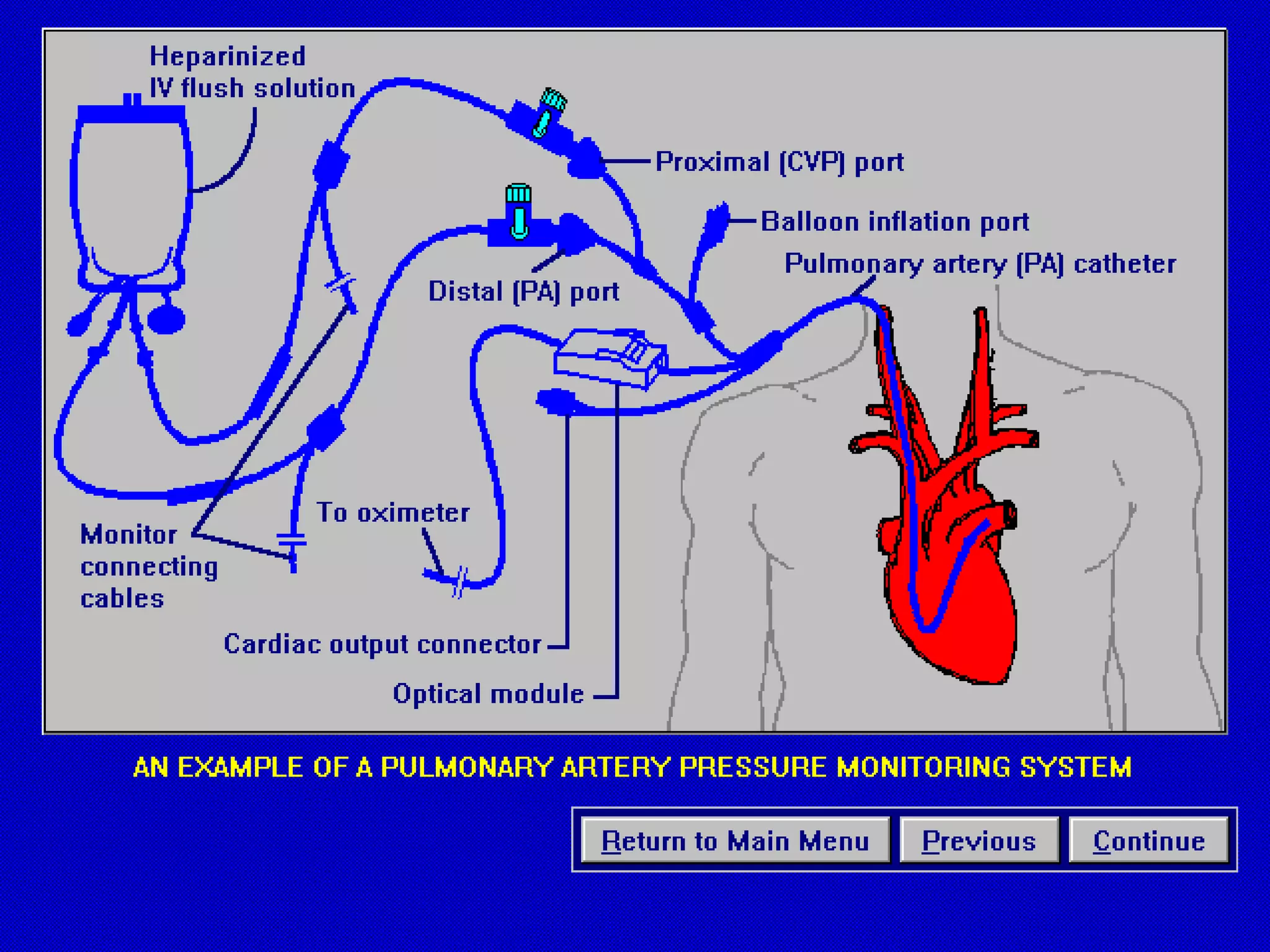
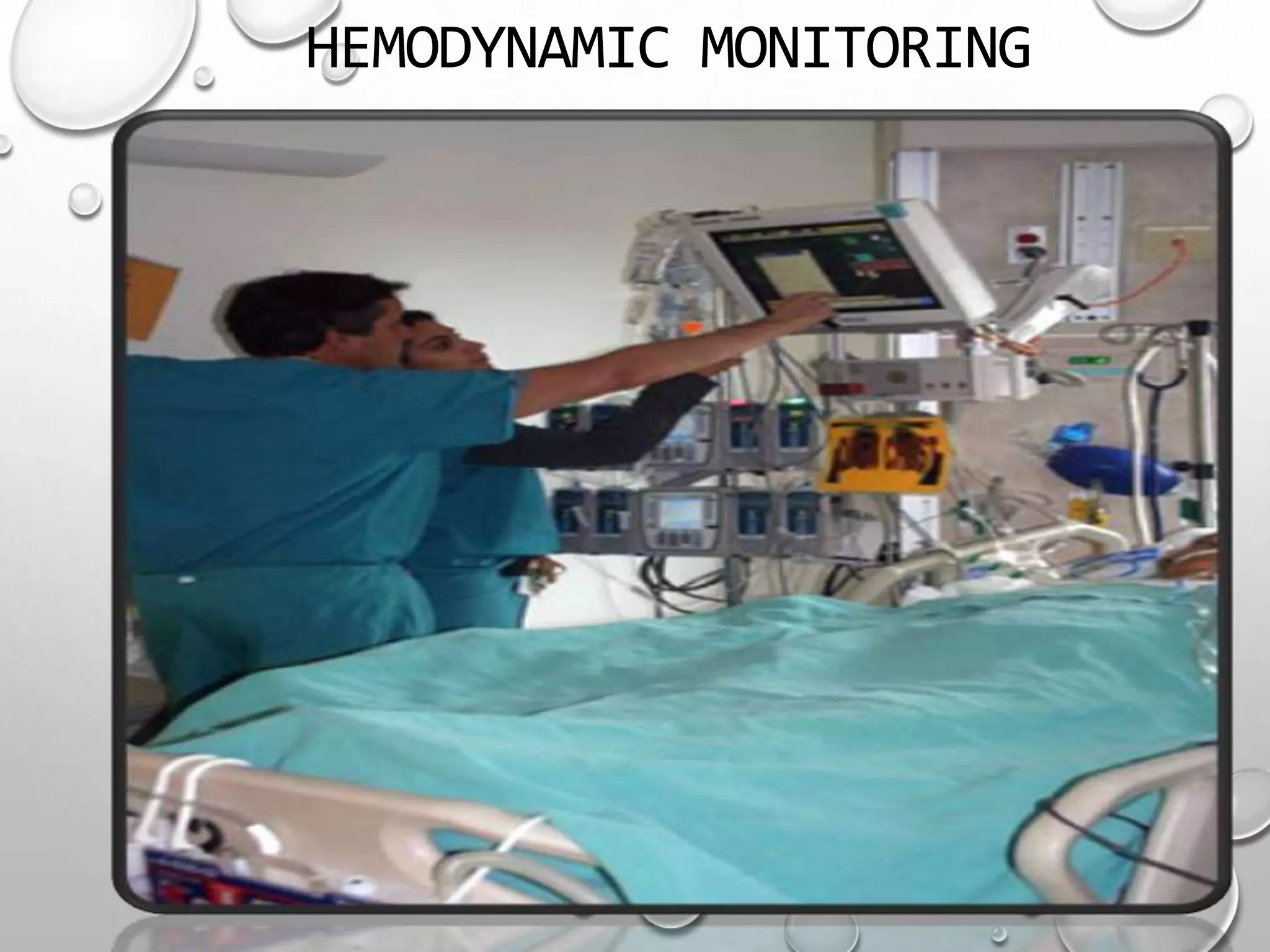
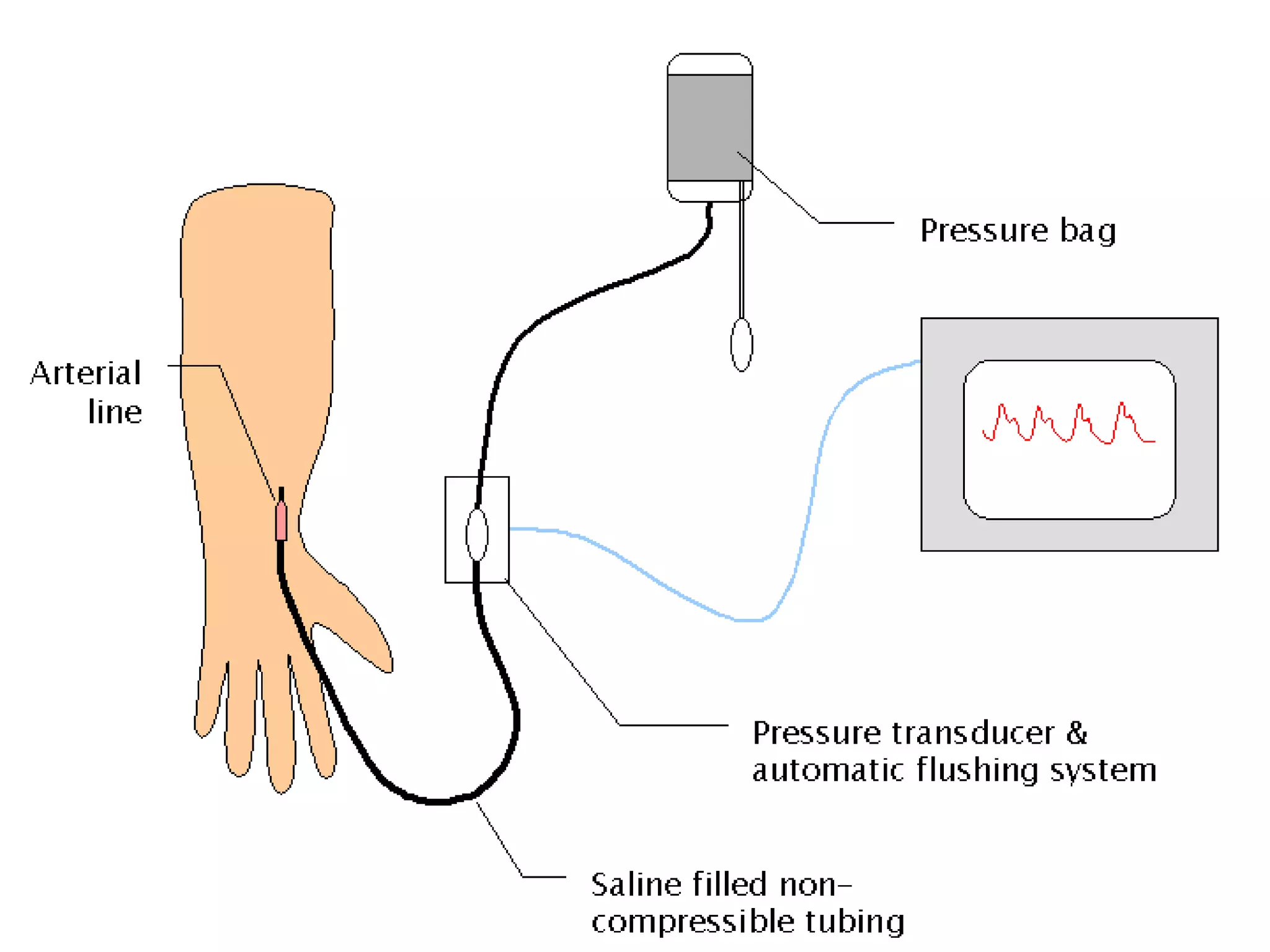
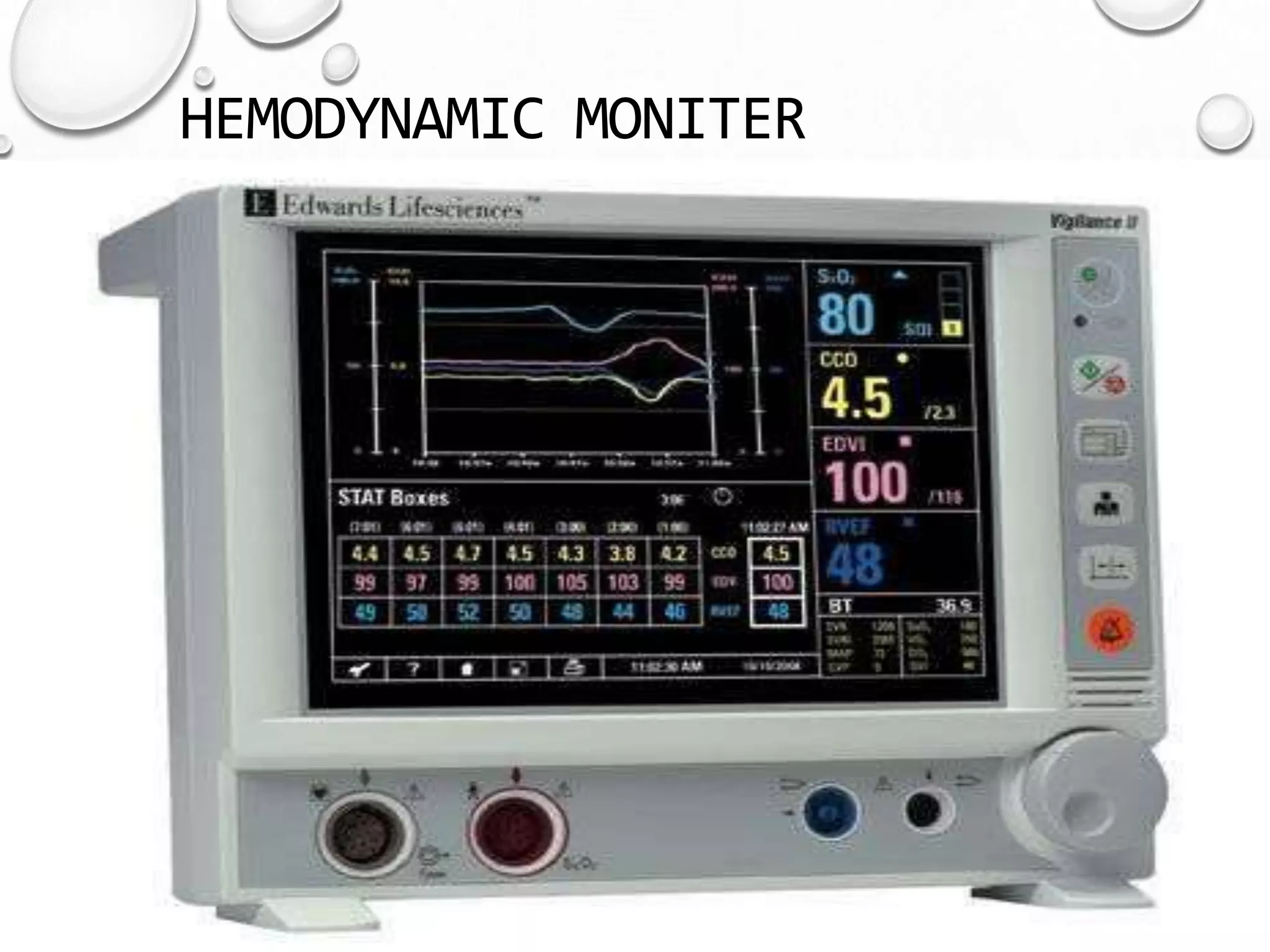
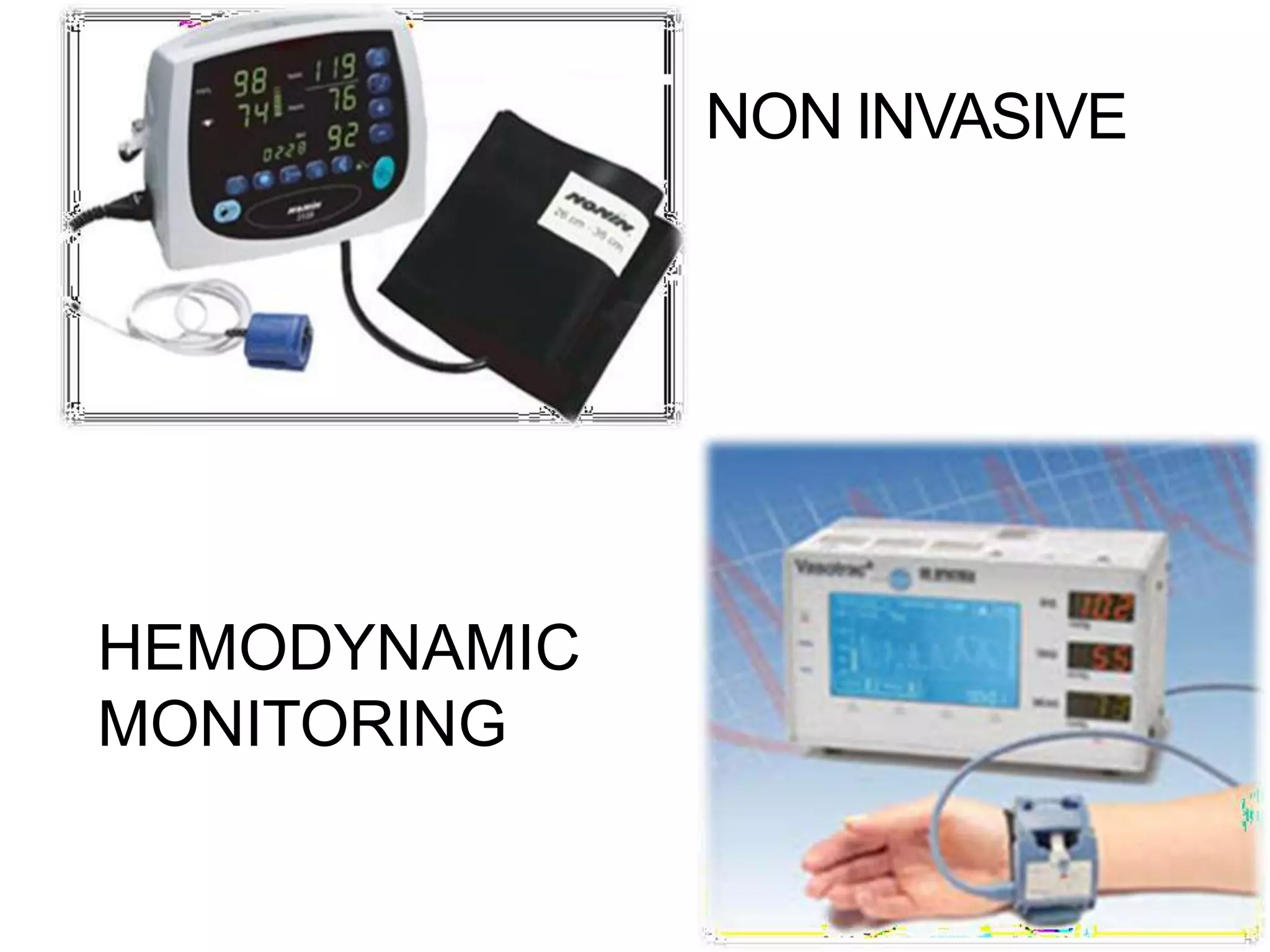
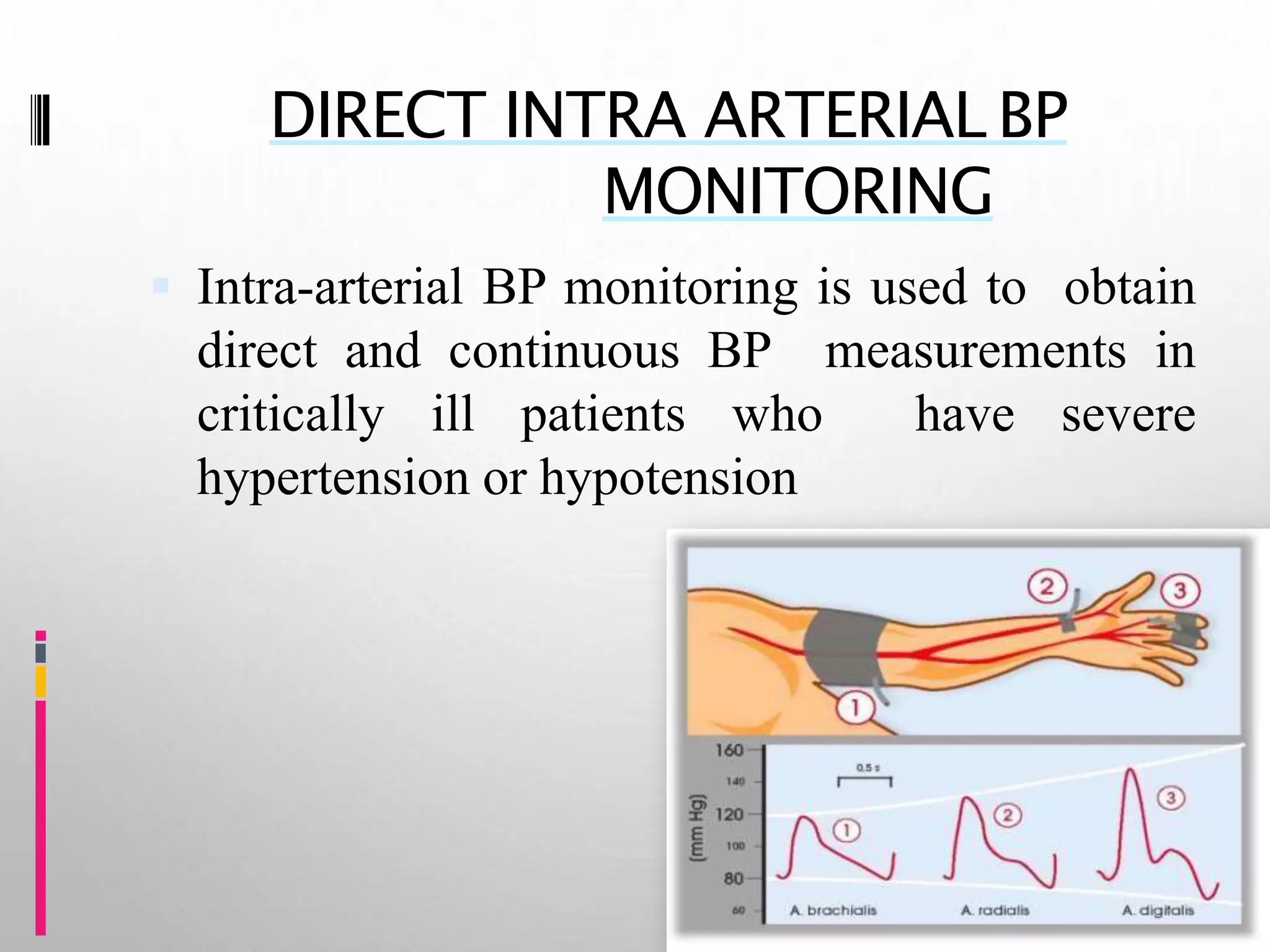
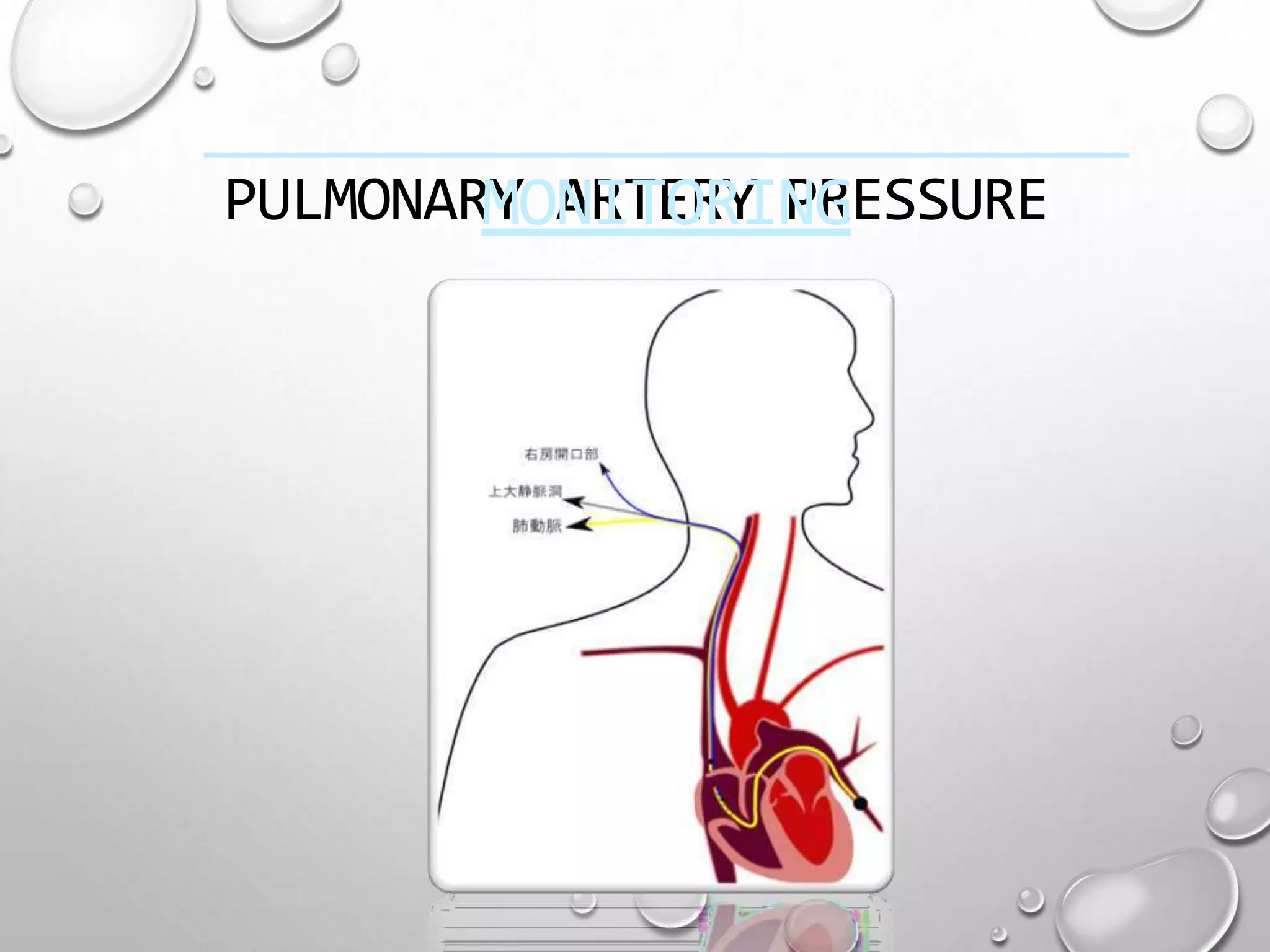
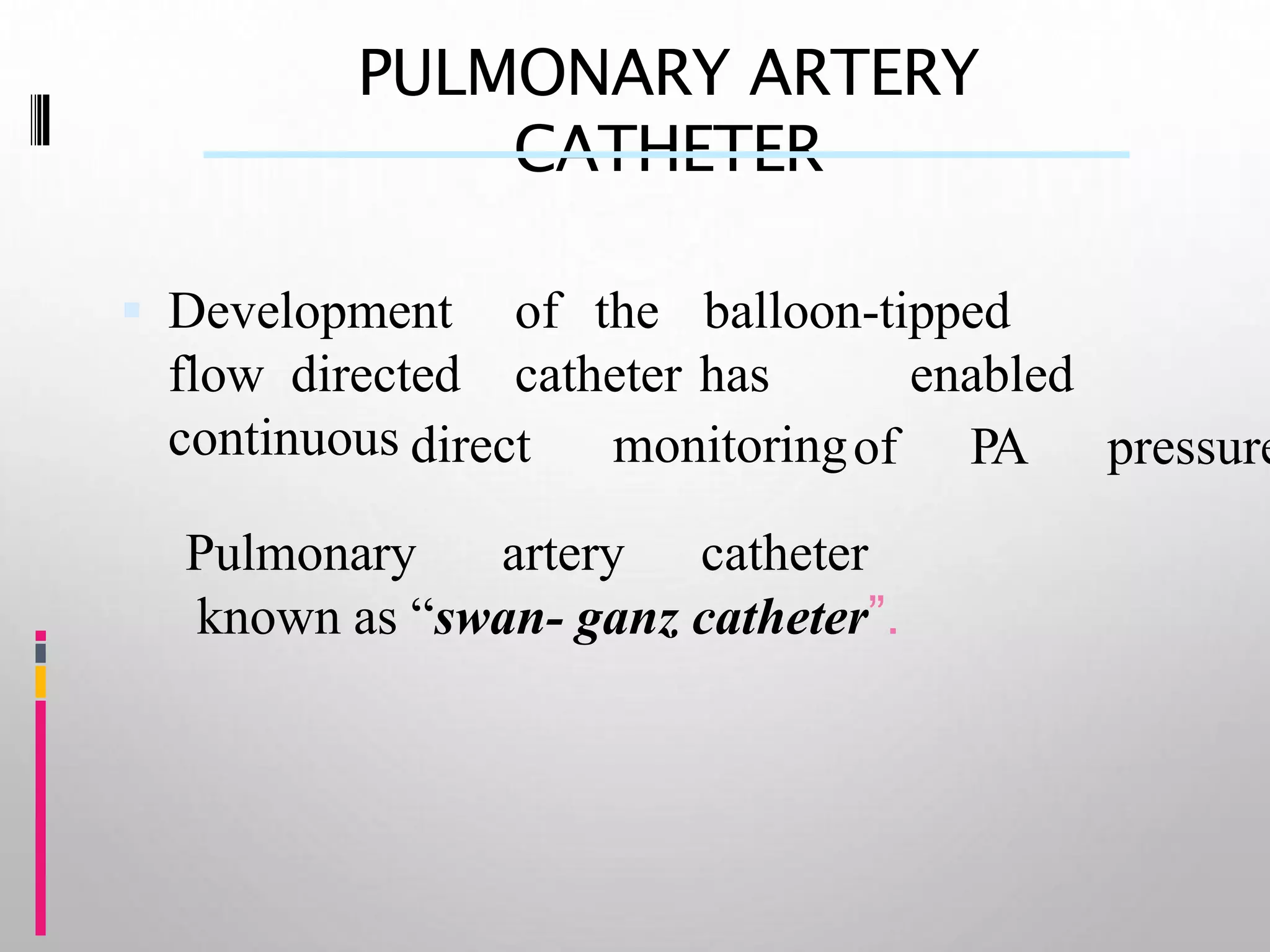
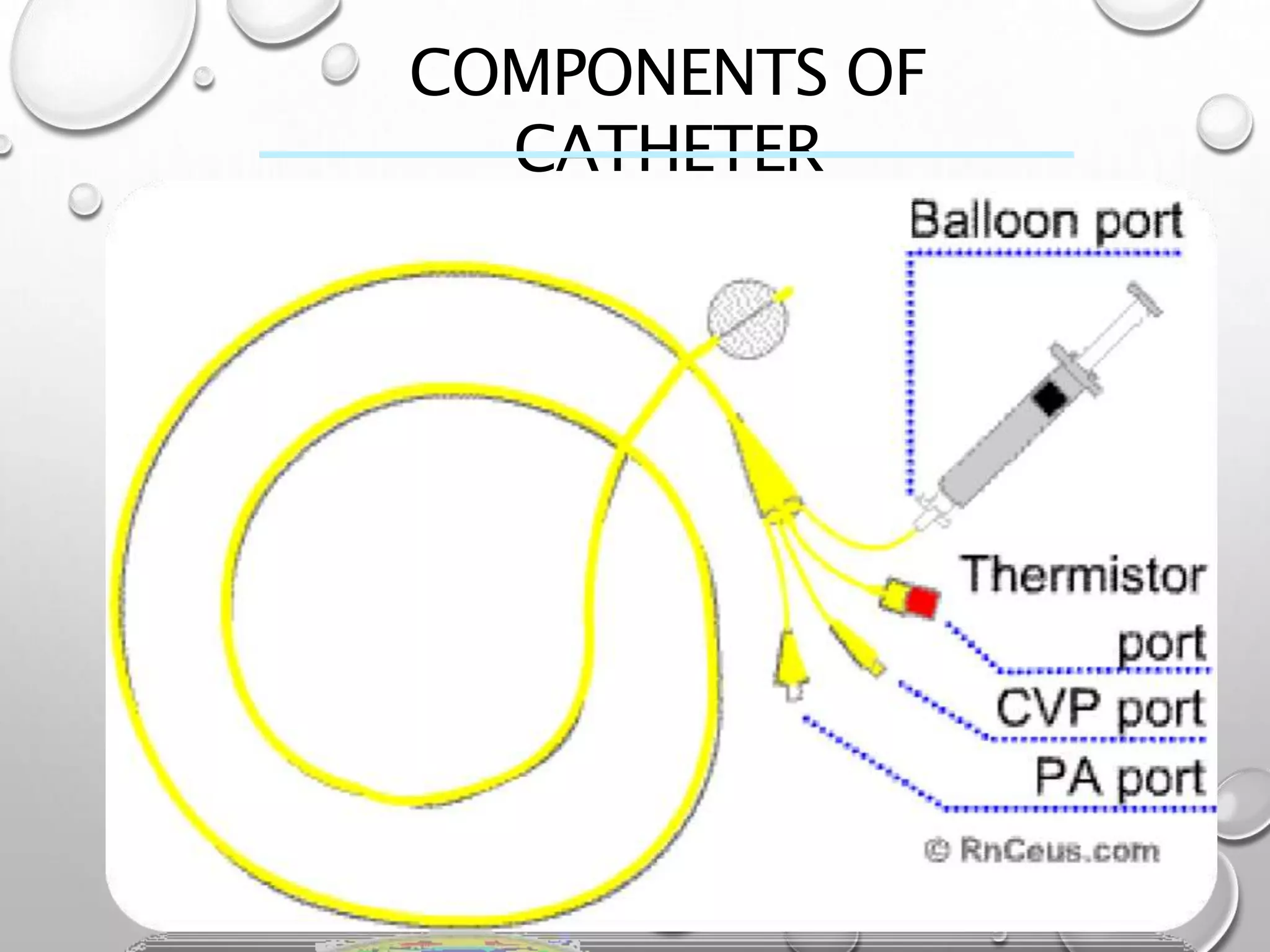
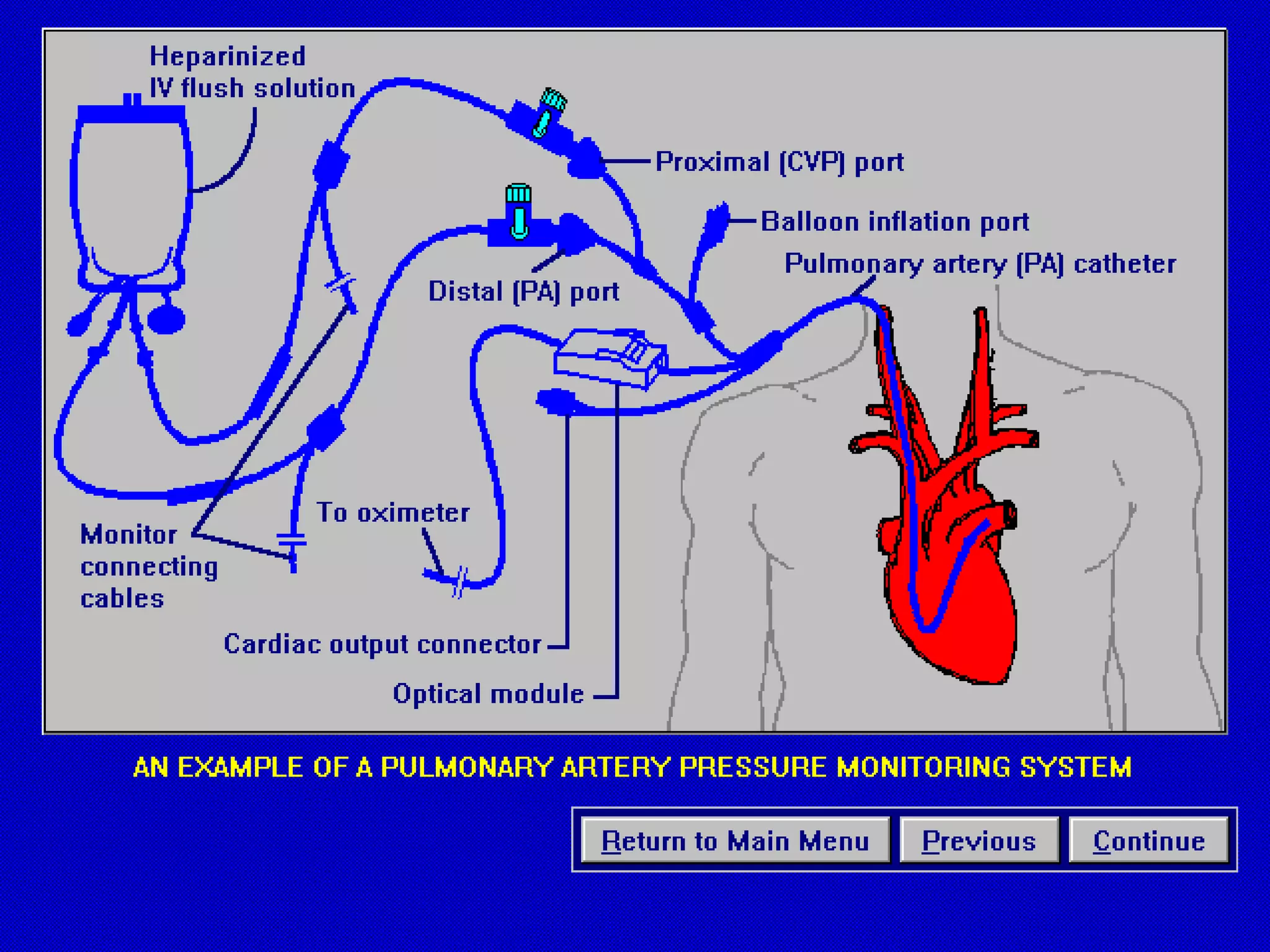
This document discusses hemodynamic monitoring, which refers to measuring the pressure, flow, and oxygenation of blood within the cardiovascular system. It is most commonly done through arterial blood pressure monitoring, central venous pressure monitoring, and pulmonary artery catheter pressure monitoring. These invasive monitoring methods provide information about how well the heart is pumping and circulating blood throughout the body. The document outlines the purposes, indications, equipment, procedures, complications, and nursing responsibilities for each of these hemodynamic monitoring methods.