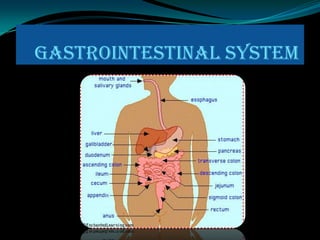
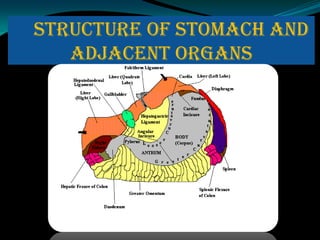
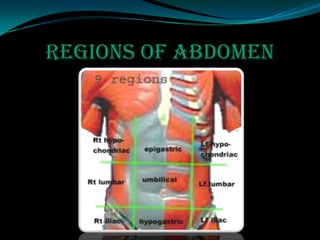
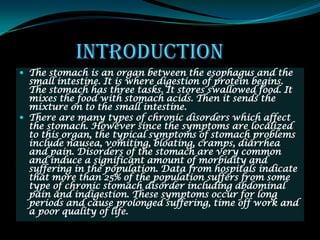
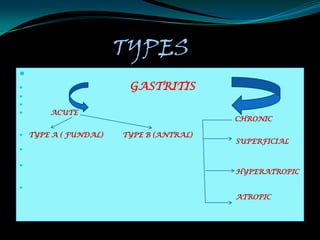
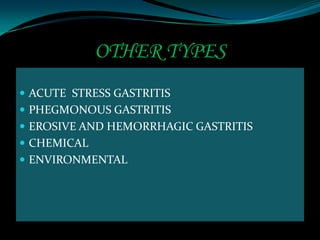
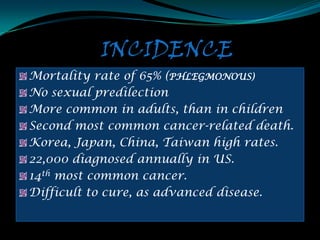
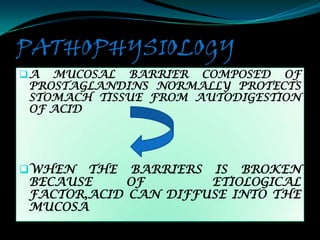
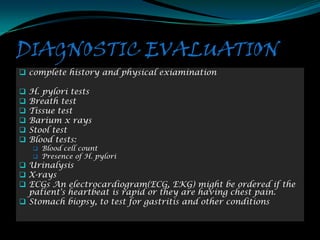
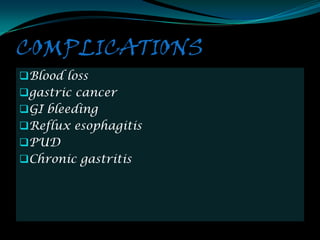
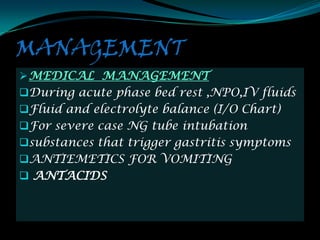
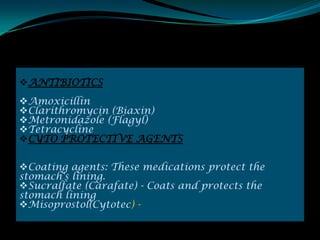
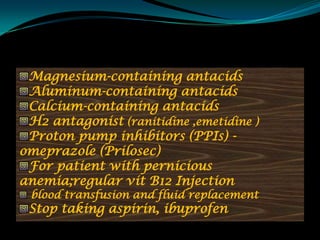
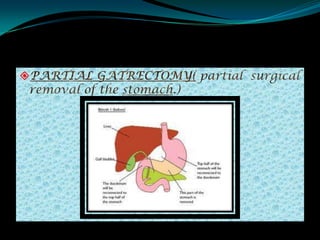
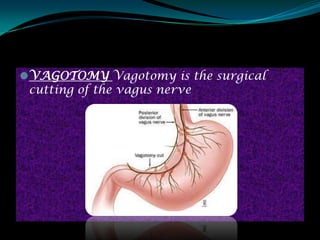
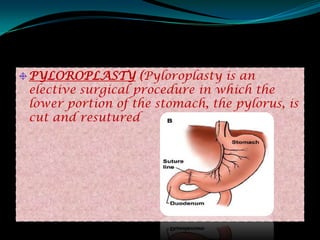
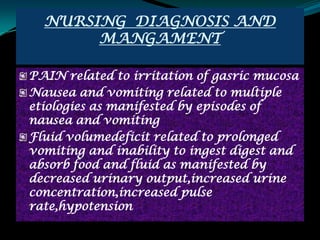
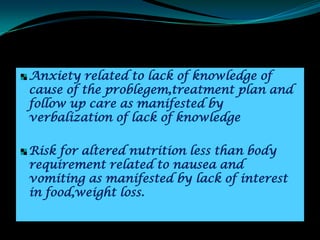
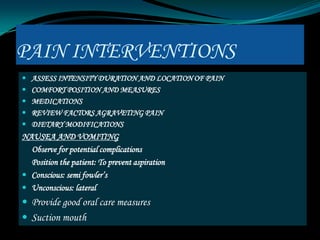
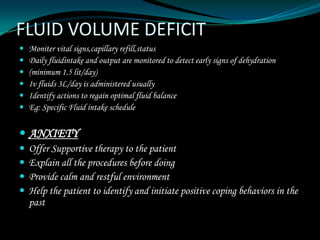
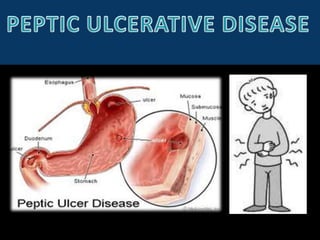
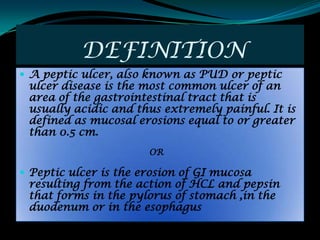
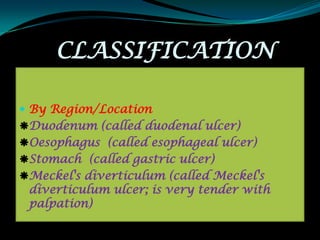
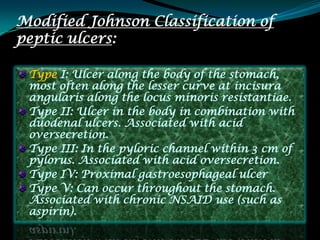
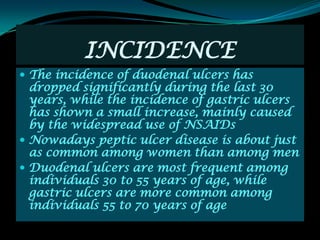
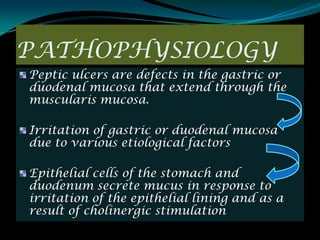
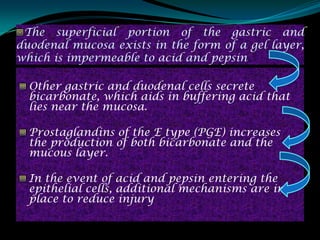
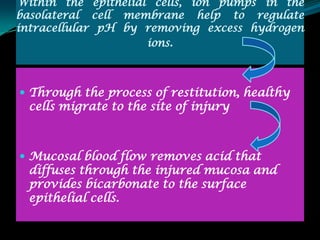
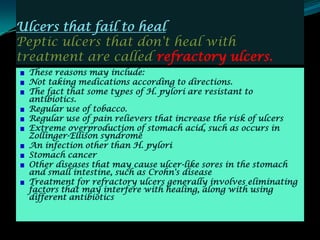
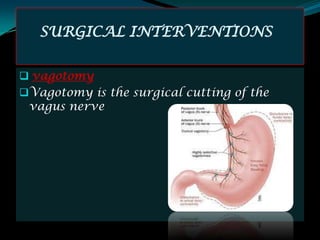
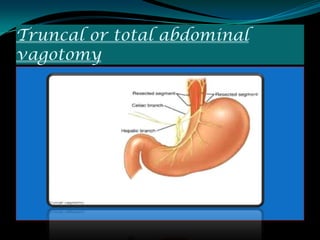
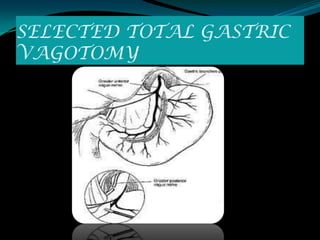
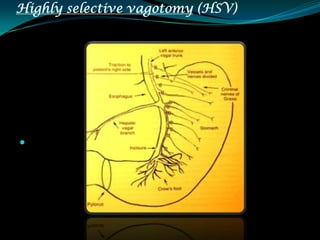
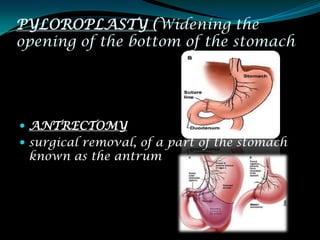
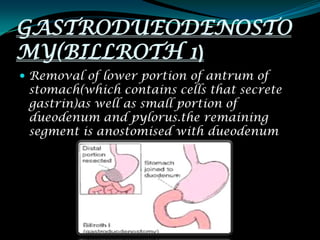
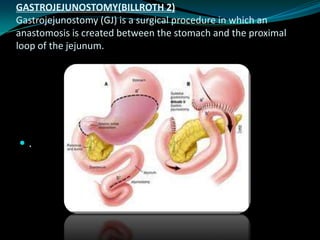
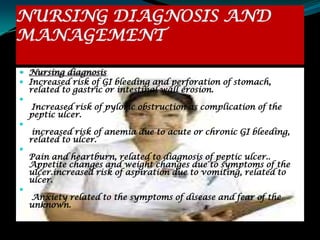
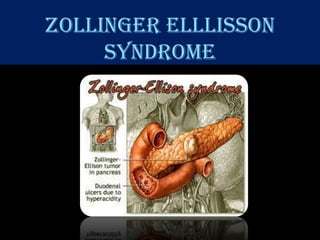
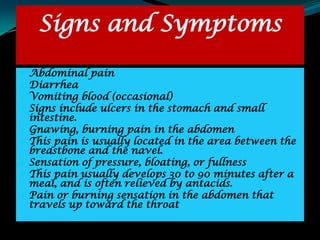
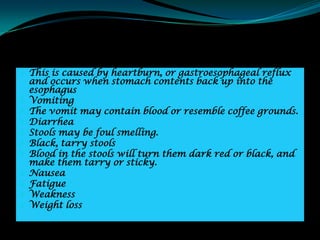
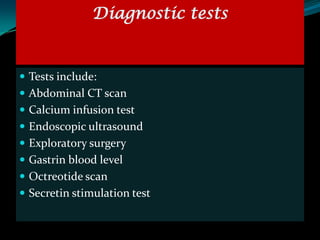
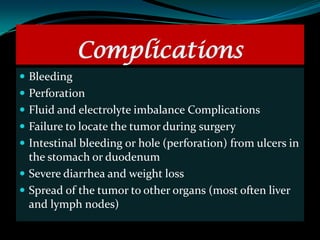
This document discusses interventions for stomach disorders including gastritis, peptic ulcer disease, Zollinger-Ellison syndrome, and gastric cancer. It begins with an introduction to the anatomy and physiology of the stomach. Gastritis is then defined and the types, risk factors, pathogenesis, clinical features, diagnostic evaluation, and management are outlined. Peptic ulcer disease is similarly defined and the classifications, risk factors, etiological factors, pathogenesis, signs and symptoms, complications, diagnosis, and medical and non-medical management are described.