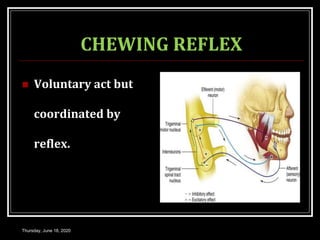
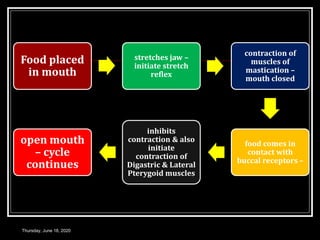
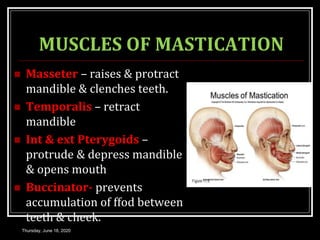
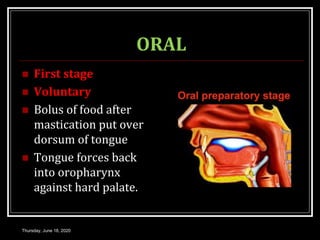
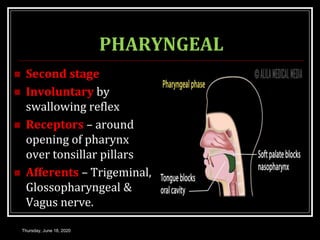
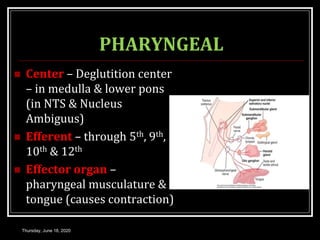
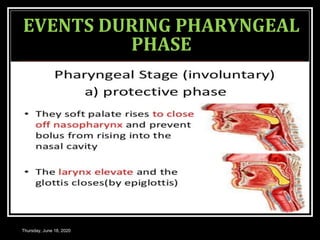
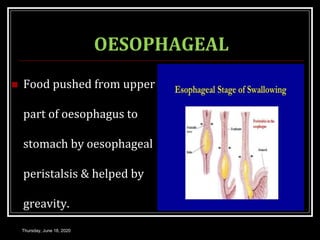
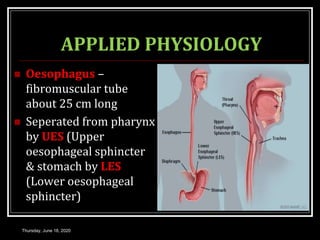
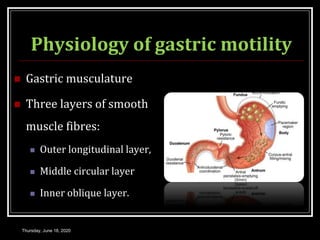
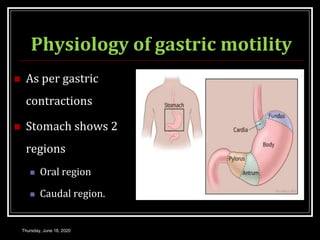
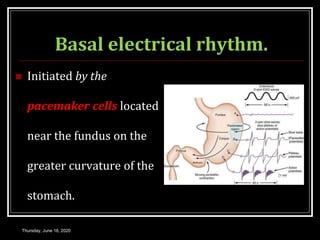
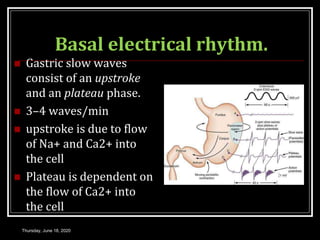
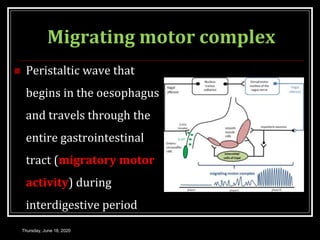
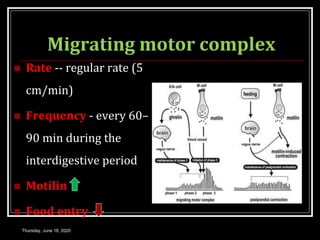
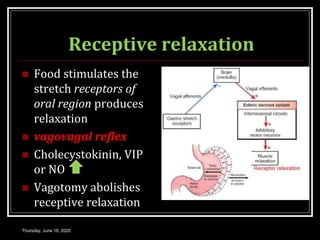
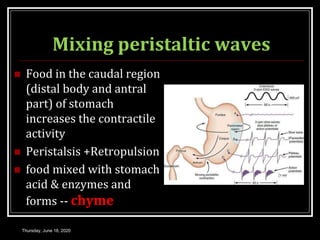
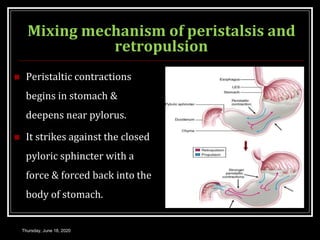
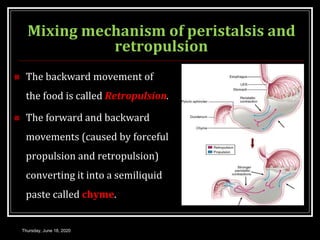
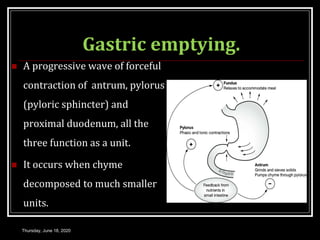
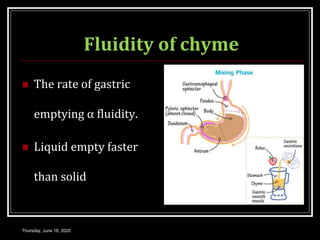
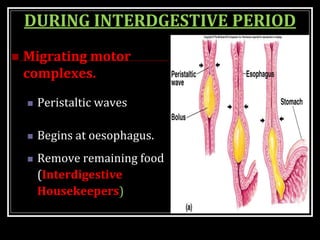
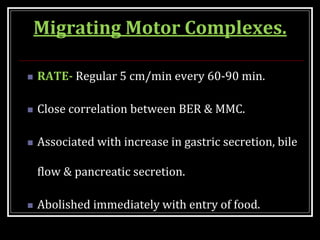
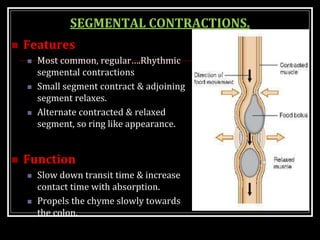
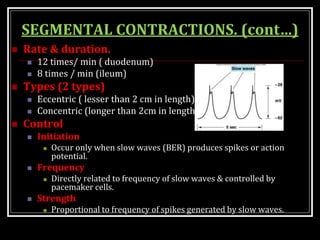
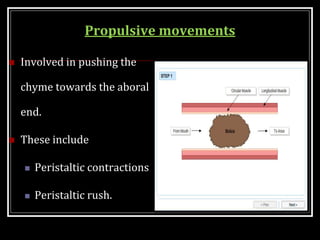
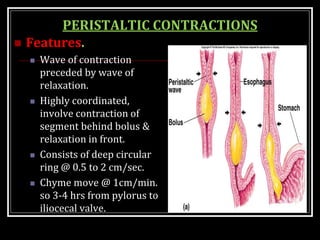
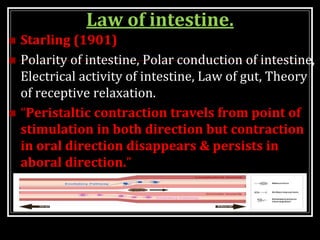
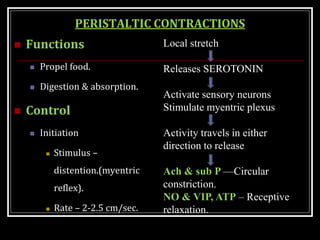
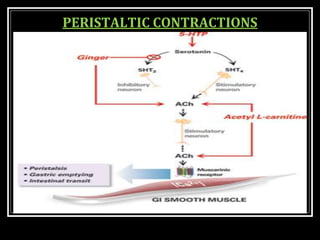
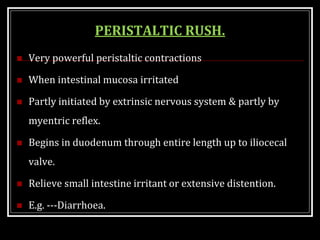
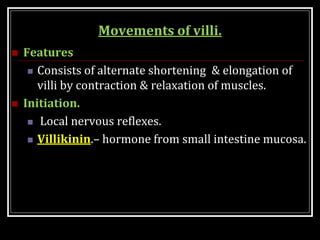
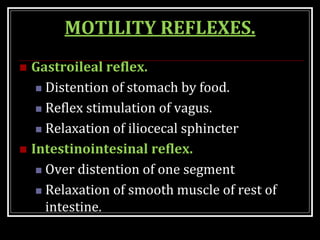
This document summarizes key aspects of gastrointestinal motility including mastication, deglutition, and gastric and small intestinal motility. It discusses the muscles and reflexes involved in chewing food and swallowing. It describes the different phases of swallowing and disorders that can occur. Motility in the stomach is summarized, including the basal electrical rhythm, factors that initiate and regulate contractions, and types of gastric movements like receptive relaxation and mixing. Small intestinal motility includes discussions of migrating motor complexes, mixing and propulsive movements like peristalsis, and the regulation of these movements.