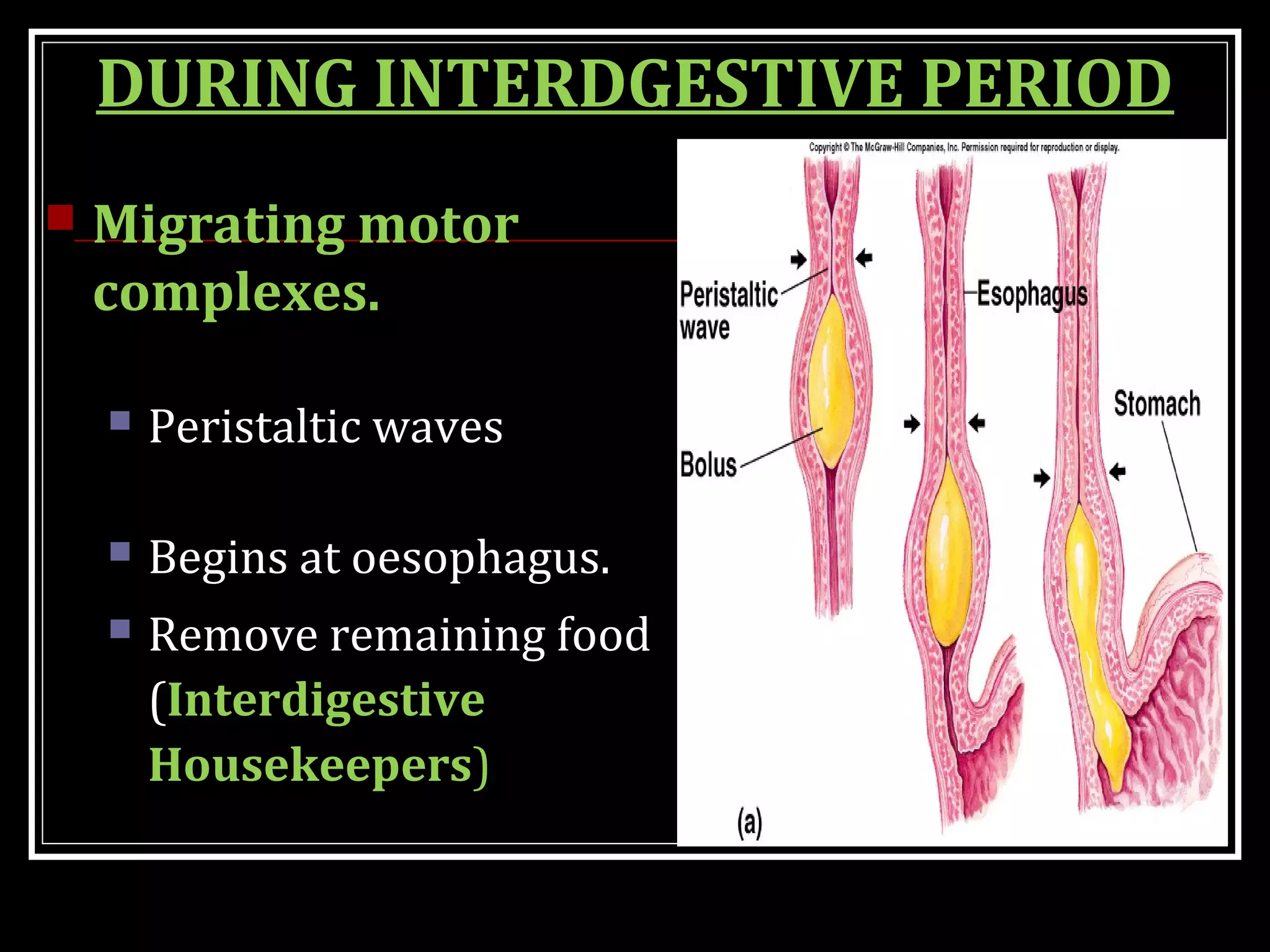
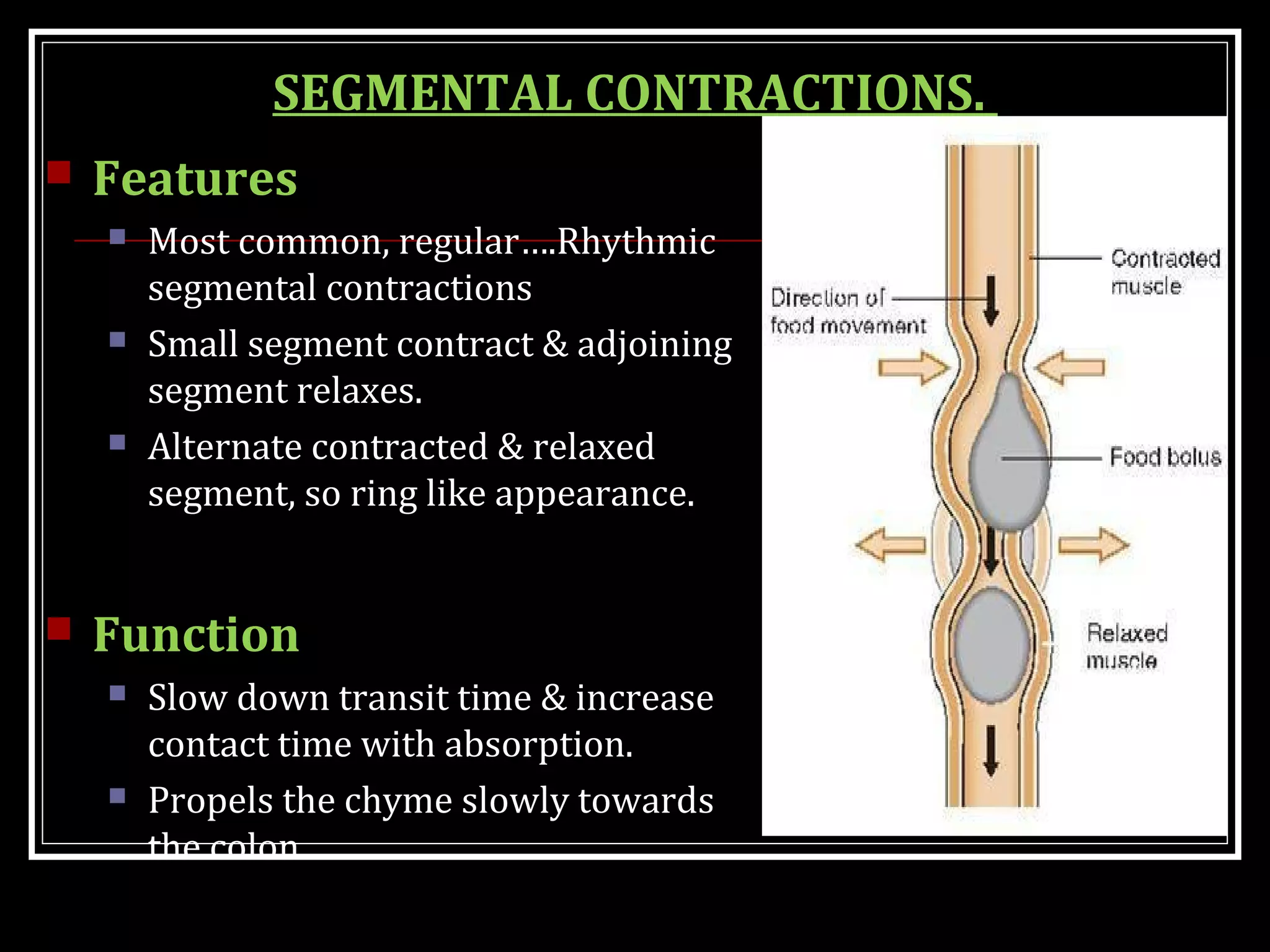
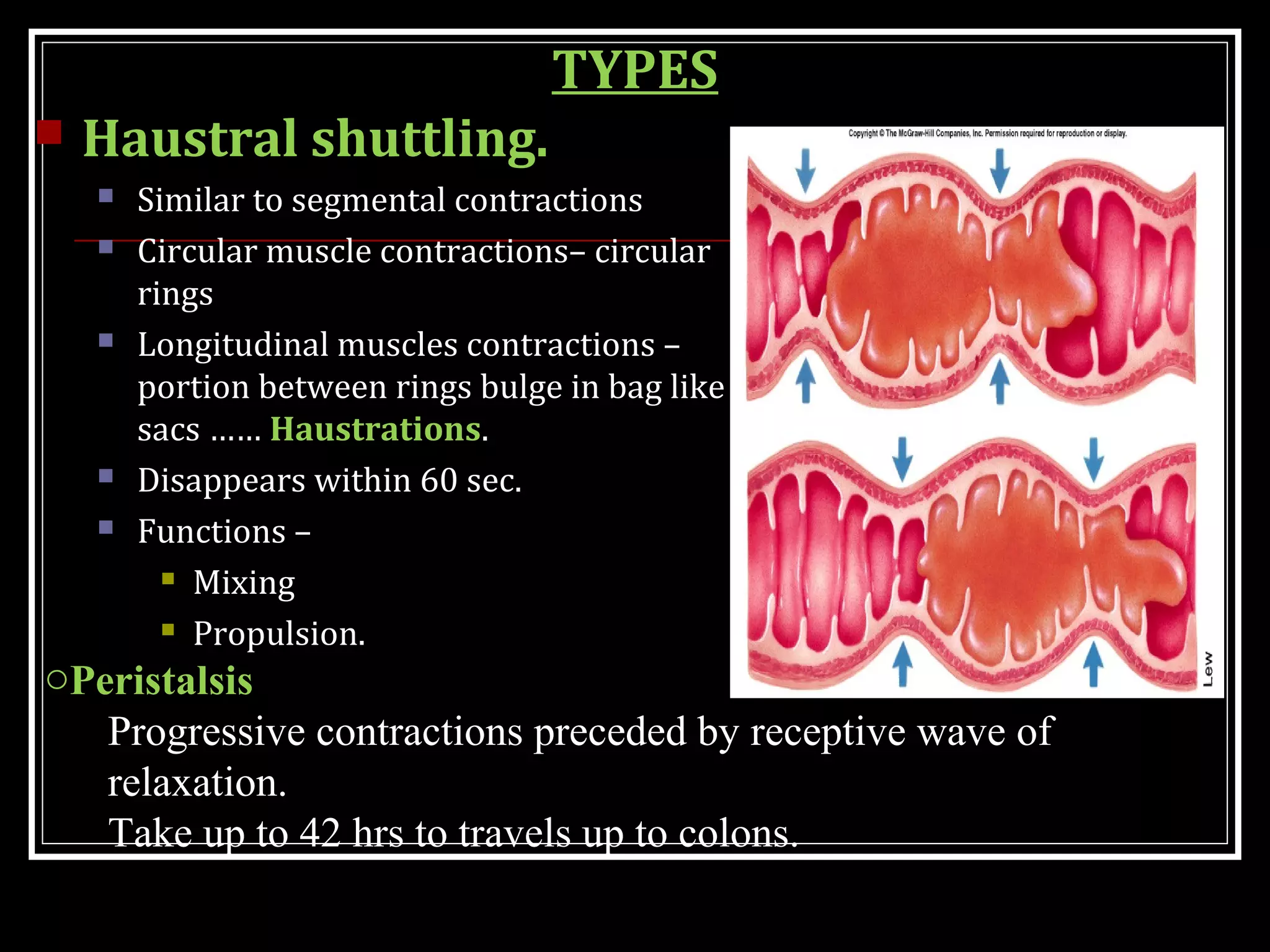
This document discusses gastrointestinal motility and the movements of the small and large intestines. It describes the different types of movements that mix and propel food through the intestines, including segmental contractions, peristaltic contractions, and migrating motor complexes. These movements are controlled by pacemaker cells and nerves. The document also covers motility reflexes, large intestine movements like haustral shuttling and mass movements, and the defecation reflex. Motility allows for digestion, absorption of nutrients, and excretion of waste from the body.