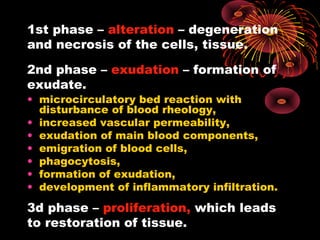
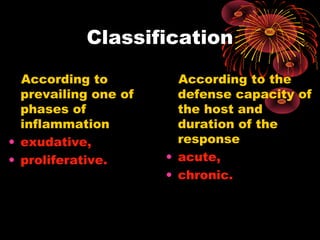
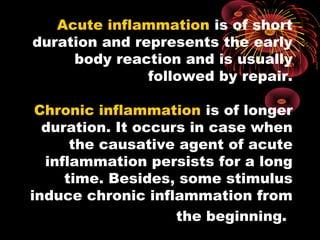
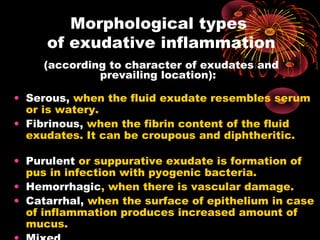
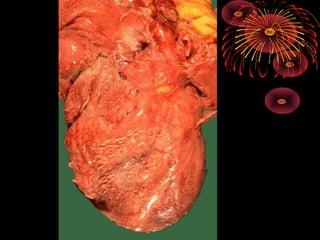
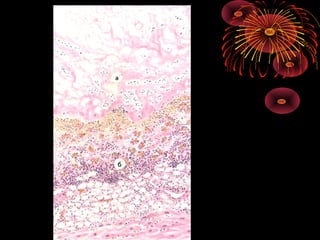
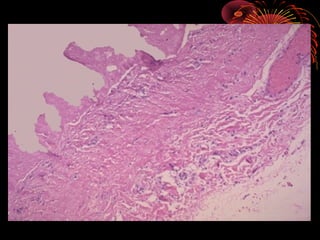
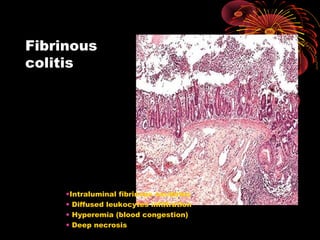
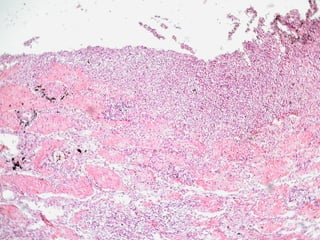
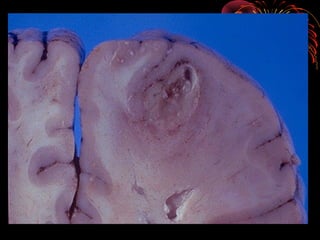
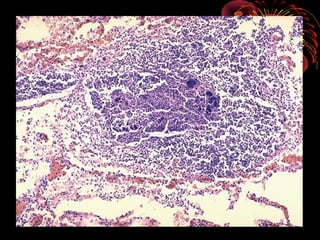
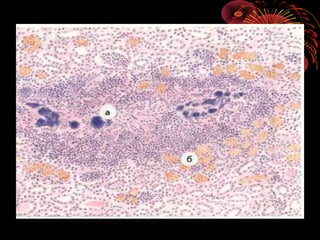
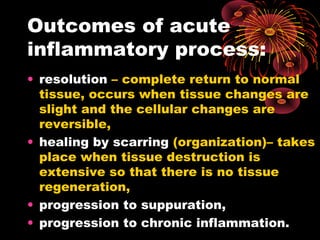
Inflammation is the body's response to injury or infection and is characterized by redness, swelling, heat, pain, and loss of function. There are three main phases of inflammation - alteration, exudation, and proliferation. The type of inflammatory response depends on factors of the organism causing it and factors of the host, and can be classified as either exudative (involving fluid exudates) or proliferative (involving cell proliferation). Exudative inflammation includes serous, fibrinous, purulent, hemorrhagic, and catarrhal types defined by the character of exudates produced and their location.