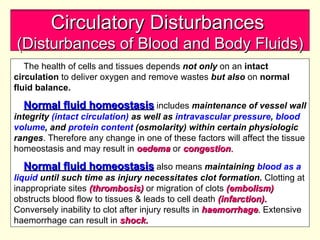
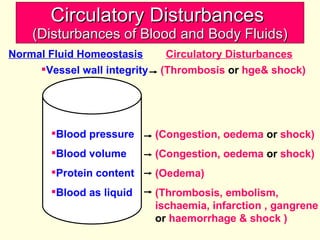
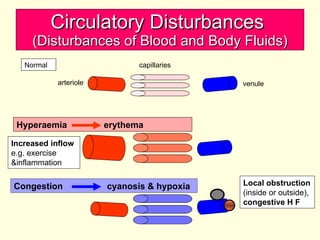
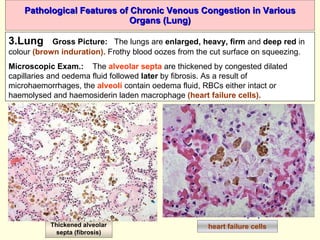
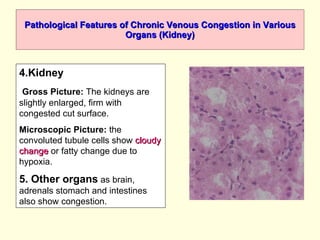
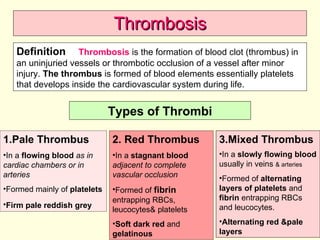
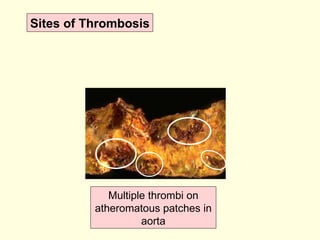
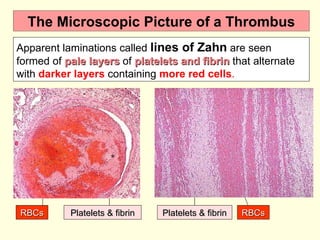
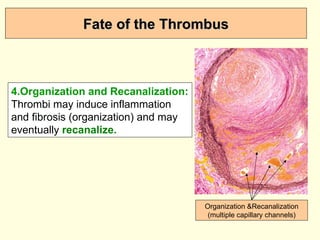
The document discusses circulatory disturbances, specifically hyperaemia, congestion, and thrombosis. It defines hyperaemia as an increase in blood flow to a tissue, which can be active via artery/arteriole dilation or passive via vein/venule engorgement. Congestion is passive hyperaemia. Thrombosis is the formation of a blood clot within a vessel and can be pale, red, or mixed depending on location and flow. Key causes of thrombosis are endothelial injury, abnormal blood flow, and hypercoagulability. Chronic venous congestion can cause organ damage over time due to increased pressure.