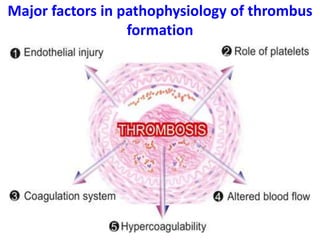
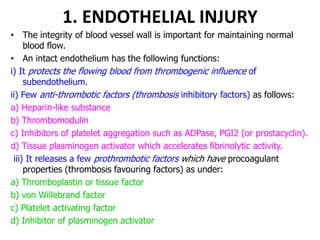
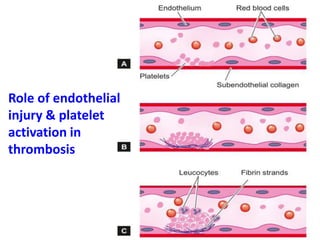
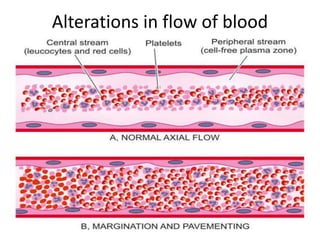
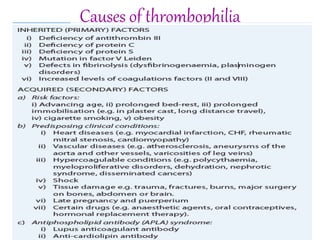
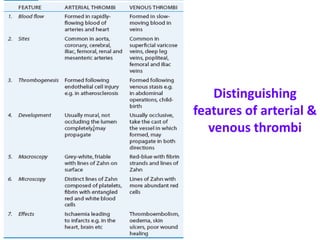
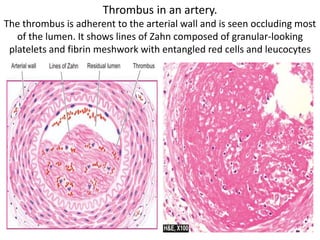
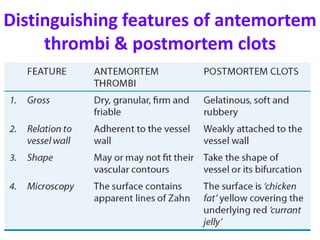
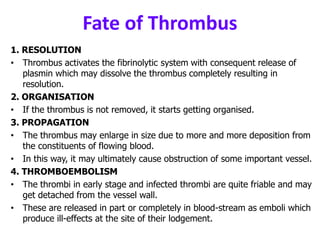
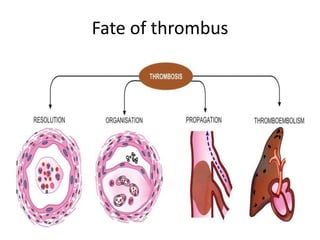
Thrombosis is the formation of a blood clot or thrombus within a blood vessel. Virchow's triad describes the key factors that predispose to thrombosis: endothelial injury, altered blood flow, and hypercoagulability. Thrombosis occurs through platelet activation and aggregation, and activation of the coagulation cascade following vascular injury. Thrombi can cause ischemic injury by blocking blood flow or thromboembolism by dislodging and blocking vessels downstream. The fate of a thrombus includes resolution, organization, propagation or thromboembolism.