1. Enterobacteriaceae are a family of gram-negative, facultatively anaerobic bacteria that include genera like Escherichia, Shigella, Klebsiella, and Salmonella.
2. They are commonly found in the intestines of humans and animals. Diseases caused by Enterobacteriaceae include urinary tract infections, diarrhea, sepsis, and meningitis.
3. Identification and classification is based on characteristics like morphology, culture properties, biochemical reactions, and antigenic structures including O, K, and H antigens. Treatment involves antibiotics but resistance is common, sometimes requiring surgery.

![ENTEROBACTERIACEAE[family]
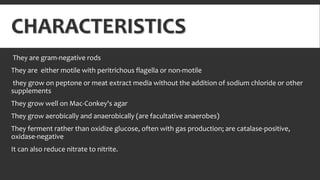
They are facultative anaerobes or aerobes .
They ferment carbohydrates, posses antigenic structures and also produces variety of toxins.
it is gram negative.
It is rod shaped.
Natural habitat is intestinal tract of human and animals.
Genera: Escherichia
Shigella
Enterobacter
Klebsiella
Serratia
Proteus](https://image.slidesharecdn.com/entero-bacteriaceae-150705131337-lva1-app6891/85/Entero-bacteriaceae-2-320.jpg)



![SHIGELLA
Shigella are nonmotile
They usually do not ferment lactose but do ferment other carbohydrates.
They produce acid but not gas.
They do not produce H2S.
The four Shigella species are closely related to E coli.
Many share common antigens with one another and with other enteric bacteria
[eg: Hafnia alvei and Plesiomonas shigelloides]](https://image.slidesharecdn.com/entero-bacteriaceae-150705131337-lva1-app6891/85/Entero-bacteriaceae-9-320.jpg)