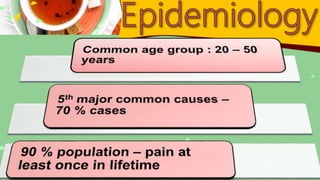
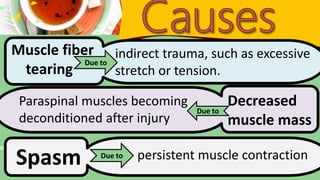
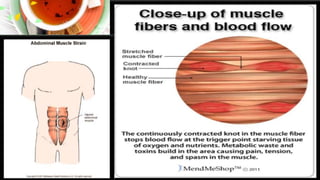
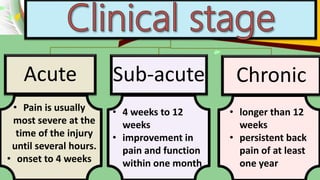
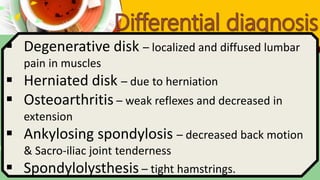
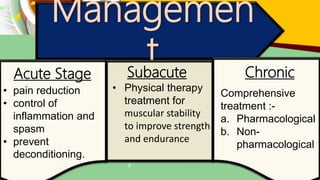
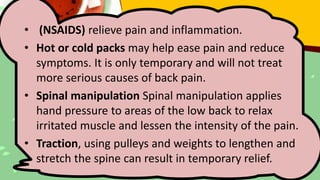
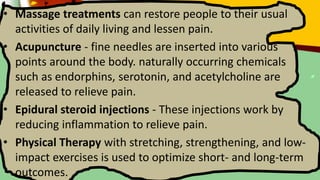
The document summarizes low back pain, including its causes, types, symptoms, diagnosis, and treatment. Mechanical stress or abnormal positioning can strain muscles and ligaments, causing acute pain. Sub-acute and chronic pain can arise from muscle tears, weakness, or deconditioning. Diagnosis involves assessing pain factors, range of motion, and ruling out other issues. Treatment depends on the pain stage and may include medications, physical therapy, exercises, spinal manipulation, massage, and injections to reduce inflammation and pain.